| Clinical Sidelights to |  |
Both the original version of Core Concepts in Anatomy, 3rd edition, and the version sequenced by dissection regions, are available on Amazon.com as Kindle books and as printed books.
Jack T. Stern, Jr.
| Clinical Sidelights to |  |
Both the original version of Core Concepts in Anatomy, 3rd edition, and the version sequenced by dissection regions, are available on Amazon.com as Kindle books and as printed books.
For those who are interested, I have created a web site that allows you to test your knowledge of radiology, including CT and MRI scans. Just click on the green rectangle.
Clinical Sidelights material added or revised during the six months prior to the last
update (August 31, 2023) appears in red. Click on the red link below to be taken directly to newly added or revised material.
Kudos to Dr. Vinod Balachandran
Endoscopic Carpal Tunnel Release
Curvatures
At birth the entire vertebral column has a gentle curve that is concave on its ventral surface (i.e., a kyphosis). This kyphosis persists in the thoracic region and in the sacrum. A lordosis (which is concave dorsally) begins to form in the neck when the child learns to lift up its head, and becomes accentuated as sitting develops. This lordosis is caused by the cervical intervertebral discs becoming taller anteriorly than they are posteriorly. A second lordosis begins to form in the lumbar region when the child learns to sit; it becomes accentuated as walking develops. The lumbar lordosis is due to the fact that both the lumbar intervertebral discs and lumbar vertebral bodies become taller anteriorly than posteriorly.
Herniated (Slipped) Intervertebral Disc
(I wish to acknowledge the very great
contribution of Dr. Michael Egnor to this section.)
Protrusion of the nucleus pulposus covered by a thin layer of stretched anulus fibrosus, or
extrusion of nuclear material through a tear in the anulus, is called a slipped or herniated disc. It
occurs most commonly in the low lumbar region. No doubt this is due to the very much greater
stresses on the discs of this region. The second most frequent site is in the neck, usually as a
consequence of some trauma. A herniated nucleus pulposus will generally protrude either to the
right or to the left of the posterior longitudinal ligament. Central herniations (i.e., those that push out in
the midline) are uncommon but do occur, more frequently in the lumbar region than in the
cervical region because the posterior longitudinal ligament is weaker in the lumbar region.
When the herniation of the nucleus pulposus is to one side of the posterior longitudinal
ligament, a common consequence is compression of a spinal nerve (sensu lato) as it is heading toward its
intervertebral foramen. Herniations of a cervical disc affect the spinal nerve that exits at the
intervertebral foramen located at the same level as the disc. Thus, herniation of the C5/6 disc may
compress the nerve that exits through the C5/C6 intervertebral foramen, which is the C6 spinal
nerve; herniation of the C7/T1 disc may compress the nerve heading toward the C7/T1
intervertebral foramen, which is the C8 spinal nerve.
The situation is different for lumbar disc herniations. Because the pedicles of a lumbar vertebra attach to the upper
half of its body, lumbar intervertebral foramina are set high relative to the
intervertebral disc. As a lumbar spinal nerve exits its intervertebral foramen, it is related more to
the back surface of a vertebral body than to an intervertebral disc. For example, the L5 spinal
nerve exits the L5/S1 intervertebral foramen along the posterior surface of the lower half
of the L5 vertebral body, which places the nerve above and lateral to a herniation of the L5/S1 disc. A herniation of the L5/S1
disc is far more likely to compress the S1 spinal nerve as it is heading downward toward its exit
from the S1/S2 intervertebral foramen. The general rule is that a slipped lumbar disc leads to
a radiculopathy (spinal nerve root disease) of the next lower spinal nerve. Thus, herniation of the L4/L5 disc may
compress the nerve that exits through the L5/S1 intervertebral foramen, which is the L5 spinal
nerve; herniation of the L5/S1 disc may compress the nerve heading toward the S1/S2 intervertebral foramen, which is the S1 spinal nerve.
The bottom line is that, whether in the neck or in the lumbar region, herniation of a disc is most likely to affect the spinal nerve with
the same name and number as the lower bounding vertebra. Lovers of anatomy will understand that the reasons for this are very
different in the two parts of the body
Specific Symptoms of Herniated Lumbar Intervertebral Discs
In the more common case of a low lumbar slipped disc, the site of nuclear protrusion or
extrusion is
inferior to the spinal cord, and only spinal nerve roots are in any danger of compression.
(If a herniation occurs in the neck, the spinal cord may also be subjected to pressure.) A central
herniation of the L4/L5 disc, while uncommon, may compress sacral nerves roots bilaterally,
producing what is called a "cauda equina syndrome", associated with difficulty urinating, fecal
incontinence, and pain or numbness in the perineum and lower limb. This requires immediate
surgery.
The most common symptoms of a slipped lumbar disc are pain in the back (possibly due to a
tear of the anulus) and pain in the body segment to which the affected spinal nerve distributes
(so-called radicular pain). Pain localized to the back, without
radiating along the distribution of a spinal nerve, is probably not due to a slipped disc, but rather
to strained ligaments or muscles of the back.
Because acute compression of a peripheral nerve does not cause pain along that
nerve's area of distribution, but rather causes paresthesia (tingling, pins and needles) followed by
numbness, some authors believe that the radicular pain accompanying a slipped disc is caused
either by compression of the dorsal root ganglion and/or an inflammatory response in the compressed dorsal root.
Among the evidence for the latter viewpoint is that local injection of
corticosteroids, which reduce inflammation, will sometimes eliminate the radicular pain. Regardless, even though the patient experiences radicular pain in the area innervated by the affected spinal nerve, actual testing of the
skin supplied by this nerve reveals diminished or
lost sensation.
The most frequently herniated lumbar discs are L4/5 and L5/S1; thus the most
commonly affected nerves are L5 and S1. For this reason it is important that you the know the
rough distributions of these nerves. The pain resulting from L5 involvement spreads from the
outer aspect of the lower leg across the dorsum of the foot to its inner border. The pain of S1
involvement is down the
calf and into the sole and outer border of the foot. The numbness associated with L5 compression
is most marked over the dorsum of the big toe. The numbness associated with S1 compression is
most marked on the lateral part of the sole of the foot.
Since a herniated disc will also compress a ventral root, motor weakness is
a common symptom. The greatest degree of motor weakness
associated with an L5 ventral root compression is that of dorsiflexion of the big toe, and to a lesser extent of the
other toes and ankle. The weakness associated with an S1 ventral root compression is predominantly one of
plantarflexion of the foot.
Compression of the L4 nerve roots is
less common than of either L5 or S1. Numbness is most marked over the medial malleolus; knee
extension (and to a lesser extent ankle dorsiflexion) is weak.
The physical exam procedure for a slipped disc is called the "straight leg raise". With the
patient lying on his/her back, you lift the lower limb on the same side as the pain that has been
reported. If radicular pain can be elicited before you have
flexed the hip through 70°, this suggests the presence a herniated disc. Since the nerve
roots don't even get stretched until you have flexed the hip through at least 30°, if the
patient complains of radicular pain early in the movement, it is a sign of something other than a
slipped disc. A positive straight-leg raise (pain arising from 30-70°) is further confirmed if
the pain gets worse when you let the leg lie flat on the table but dorsiflex the ankle. You should
also try to raise the lower limb on the side opposite to that on which the patient has reported pain.
Although a contralateral straight leg raise does not typically produce the radicular pain of a slipped disc,
if the pain does occur, it is even more diagnostic of a slipped disc than is a
positive ipsilateral straight leg test. When a contralateral straight leg raise test is positive, the herniated
nucleus pulposus is probably pressing into the acute angle between the spinal nerve and the dural
sac (the so-called axilla of the spinal nerve). Spondylolysis and Spondylolisthesis
The superior surface of the S1 vertebral body is tilted to face partly forward. As a result,
body weight pushing down on the L5 vertebra should cause it to slip downward and forward off
of S1. While this is resisted by the anterior and posterior longitudinal ligaments, the IV disc, and the iliolumbar
ligaments (which run from the transverse processes of L5 to the ilia), the most important factor
preventing antero-inferior slippage of L5 is the orientation of the L5/S1 zygapophyseal joints.
This is revealed by cases in which trauma to the 5th lumbar vertebrae causes each lamina to be fractured across its "pars interarticularis" region, i.e., the region of the lamina between the origins of the superior and inferior zygapophyses. If such a bilateral pars interarticularis fracture occurs, the 5th lumbar vertebra will then be in two pieces.

Occipital Neuralgia
Neuropathy is the term that refers to any disease affecting the nervous system, though in common usage it refers specifically to a disease affecting one of more peripheral nerves. Radiculopathy, discussed above, is a kind of neuropathy. Lots of things cause pain (e.g., a punch in the stomach, or a heart attack), but if the pain is caused by a disease of peripheral nerves, it is called neuropathic pain. If the neuropathic pain is experienced along the distribution of a specific nerve, it is called a neuralgia. Patients suffering a neuralgia use such terms as burning, or stabbing, or shooting, or like an electric shock to describe the pain. In many instances the
episodes of severe pain come on quite suddenly (i.e., are paroxysmal). These episodes are usually brief (on
the order of minutes, not hours), but sometimes there is an underlying less severe pain that is
more or less constant. An episode of neuralgia may be triggered by a normal stimulus to the
region supplied by the nerve.
Occipital neuralgia is paroxysmal severe pain (bilateral or unilateral) occurring in the area of
the scalp supplied by the greater occipital and lesser occipital nerves (the latter nerve being something
you won't see until you dissect the anterior neck). These two occipital nerves carry axons of the C2 spinal nerve. Some
authors describe occipital neuralgia as being a rare condition, others say it is common. It may
have more than one cause: trauma that injures the C2 spinal nerve or its dorsal root, disease of
the lateral atlanto-occipital joint, spasm of the semispinalis capitis through which greater
occipital nerve passes, entrapment of the greater occipital nerve by the cranial trapezius through
which it may also pass. In a significant proportion of cases the neuralgia is idiopathic (i.e.,
its cause cannot be found).
Occipital neuralgia is diagnosed by injecting local anesthetic around the greater occipital
nerve. If the neuralgia disappears, the diagnosis is made. Injection may be done where the nerve pierces the fascia between the cranial trapezius and
sternocleidomastoid (or in people wide origins of the cranial trapezius, the muscle itself). This site is located on average
3½ cms inferolateral to the external occipital protuberance (Ashkenazi A, Levin M. 2004
in Postgrad Med 116(3):16-32,48), although a recent study (Natsis K et al. 2006
Occipital neuralgia is often treated with oral medications, but these may not work. While I have said that
anesthetizing the greater occipital nerve is a primary method of diagnosing occipital neuralgia, it
also serves as a treatment that lasts several weeks, and can be repeated. Other treatments include
implanting near the nerve an electrode that chronically stimulates it (presumably you will learn
why this works in your neurobiology course), or even surgical destruction of the C2 dorsal root. There Are More Things in Autonomic Heaven and Earth Than are Dreamt of in Our Philosophy
In Essentials of Gross Anatomy (p. 32 of the 2001 version, pp. 35-36 of the 2003 version), I mentioned that the sympathetic nervous system is not confined to innervation of smooth muscle, cardiac muscle, and glands, as my prior discussion of this topic would have suggested. I cited evidence that the sympathetic nervous system may influence striated muscle function (see also Khan MM et al. 2016 Sympathetic innervation controls homeostasis of neuromuscular junctions in health and disease. PNAS 113:746-750) and bone metabolism (see also Elefteriou F 2018 Impact of the autonomic nervous system on the skeleton. Physiol Rev 98:1083-1112). I have recently come across a paper stating that after cerebral ischemic injury (i.e., stroke) there occurs an increase in sympathetic tone, with attendant release of norepinephrine into bone marrow that stimulates hematopoetic stem cells to produce neutrophils and monocytes (Courties G et al. 2015 Ischemic stroke activates hematopoetic bone marrow stem cells. Circ Res 116:407-417). It is unclear if this is a beneficial or harmful response. As far as I am concerned, it is just another instance of the autonomic nervous system being far more complex than you can be expected to learn in a first-year gross anatomy course.
Sacral Autonomics May Be Sympathetic, Not Parasympathetic
This is not really a clinical sidelight, but it is so interesting that I want to bring it to your attention. It would seem to demand a revision of certain statements both in Core Concepts and in Clinical Sidelights, but I am holding off on that for now.
I and every other anatomist, neurobiologist, and physician learned that the preganglionic autonomic cells in the intermediolateral region of the sacral spinal cord are part of the parasympathetic system. In November 2016 there appeared a paper (Espinosa-Medina I, et al. 2016 The sacral autonomic outflow is sympathetic. Science 354:893-897) showing that in mice these cells, during their development and afterward, express genes that are also expressed in thoracic preganglionic sympathetic cells but not in cranial nerve parasympathetic preganglionics. Genes expressed in the latter are not expressed in sacral preganglionic cells. Further, all pelvic minute autonomic ganglia, some now said to be sympathetic and others parasympathetic, express the same genes as are expressed in sympathetic ganglia elsewhere in the body. Either mice neurons are very peculiar, or we must accept that sacral autonomics are part of the sympathetic nervous system. This wouldn't be the end of the world. It is known that some sympathetic pathways are vasoconstrictive and others vasodilatory, even to the same structure (Jänig W. 2006 The Integrative Action of the Autonomic Nervous System. Neurobiology of Homeostasis. Cambr U Press, Cambridge). Therefore, we should be prepared to accept that sacral sympathetics to pelvic structures may perform functions opposite to those performed by thoracolumbar sympathetics to these same structures. It also means that visceral sensory fibers running centrally in pelvic splanchnic nerves are following sympathetic pathways in reverse, just as visceral sensation elsewhere in the trunk. Spinal Injuries
First, in order to predict the neurologic consequences of penetrating wounds to the back, one
must know where the different spinal cord segments lie in relation to the vertebral column. There
is a relatively simple guide to this information--only the digit 1 need be memorized:
The top of spinal cord segment C1 lies opposite top of vertebra C1. It is obvious that the cervical cord is virtually unshortened relative to the vertebral column.
The thoracic cord is shortened slightly. The lumbar segments of the cord run from the top of T11
to the top of L1 and are thus shortened considerably. The five sacral and one coccygeal segments
of the cord span only the distance occupied by the body of L1.
An injury to the spinal cord not only leads to paralysis of the muscles supplied by the ventral horn of the
damaged region, it also leads to loss of cerebral control over muscles innervated by any intact
cord segments below the injury, and, of course, it prevents sensory information that enters such
intact segments from reaching consciousness. Intraspinal reflexes below the injury are unaffected
or, in the case of the stretch reflex of striated muscles, even accentuated. An injury to the spinal
cord above the L1 vertebra will remove descending influences on the sacral cord motoneurons
controlling the striated muscles that regulate urination and defecation. However, such an injury will
not affect the intraspinal parasympathetic reflexes initiating these behaviors. Thus, the bladder
contracts when it is full, generating high intravesical pressure. However, the striated muscle that
normally is responsible for the voluntary control of urination, being deprived of descending
neural influences, becomes spastic and cannot properly relax. Urination is incomplete and a suite
of complications results. It may be necessary to cut the striated muscle, or its nerve, so that the patient's bladder more
completely empties. I do not know if a similar problem characterizes defecation or
if it simply occurs automatically when visceral sensory neurons detect a full rectum. A man who
has suffered a spinal cord injury above the sacral levels of the cord can reflexly achieve an
erection (which is the result of parasympathetic discharge from S3 and S4) upon sensory stimulation of the
penis. For years I taught that a man with such an injury cannot achieve erection when shown erotic pictures, but I recently read that there is a sympathetic pathway originating in the thoracolumbar spinal cord that causes dilatation of artrioles in the corpus cavernosum, thereby duplicating the parasympathetic action causing erection (Kuhn RA 1950 Functional capacity of the isolated human spinal cord. Brain 73:1-51; Root WS, Bard P 1947 The mediation of feline erection through sympathetic pathways with some remarks on sexual behavior after deafferentation of the genitalia. Am J Physiol 151:80-90). This allows a psychogenic erection in a man whose spinal cord was transected between L2 and S3, and also in a man whose sacral cord was itself severely damaged. In addition to these thoracolumbar sympathetic neurons promoting penile erection, there are other thoracolumbar sympathetic neurons that cause constriction of penile arterioles and consequent detumescence.
It should be obvious that injuries to the vertebral column below the L1/L2 intervertebral disc
only pose a risk to spinal nerve rootlets, not to the spinal cord itself. Lumbar Puncture
Because the subarachnoid space inferior to the L1/L2 disc is filled with dorsal and ventral
rootlets floating in a pool of cerebrospinal fluid, a needle inserted between spines of the lower
lumbar vertebrae, and then through the dura/arachnoid into the subarachnoid space, will not injure the spinal
cord unless the cord extends further inferiorly than is typical (there being some normal variation in how far down the spinal cord
goes). Just as one would find it difficult to impale a piece of cooked spaghetti floating in water, so
a needle inserted between low lumbar spines into the subarachnoid space will likely just push floating
rootlets aside. Such a procedure is called a lumbar puncture. The needle must pass
through the supraspinous ligament, interspinous ligament, ligamentum flavum (which is often
perceived as offering greater resistance), epidural space, dura, and arachnoid. Lumbar punctures that enter the subarachnoid space are done to sample cerebrospinal fluid or to inject anesthetic agents into the CSF. The tip of the needle may be stopped at the spinal epidural space for the purpose of injecting anesthetic agents here (see Lumbar Epidural Anesthesia below).
In the adult, the preferred site of a lumbar puncture is between the 3rd and 4th lumbar spines because this site is sufficiently low to avoid the spinal cord in almost everyone. A lumbar puncture may be attempted between the spines of L2 and L3 (but see below), or less commonly between L4 and L5. Regardless, if the patient is asked to adopt a position with the lower back flexed, the space for passage of the needle between any two adjacent spines is widened. It should be obvious that a pregnant woman near full term cannot flex her lumbar spine as much as most other people. Identification of the chosen interspace relies on the knowledge that the 4th lumbar spine is palpable in the posterior midline of the back at the site where it is
crossed by the supracristal plane, but again, there is variation between individuals in the position of the supracristal plane relative to the vertebral spines. A recent study of epidural anesthesia for control of labor pain, and of spinal anesthesia for Caesarian section, compared anesthesiologists' estimates of what interspace they had entered to identification of the actual interspace by ultrasound (Whitty R, Moore M, Macarthur A. 2008 Identification of the lumbar interspinous spaces: palpation versus ultrasound. Anesthesia & Analgesia 106:538-540). The estimates were correct only 55% of the time, with the greatest proportion of errors being entry one interspace higher than what the anesthesiologist had believed. This study supports the conclusion of an earlier report (Reynolds F. 2001 Damage to the conus medullaris following spinal anesthesia. Anaesthesia 56:235-247) that "Given the inaccuracy of methods of identifying lumbar interspaces, and the variability of the position of the conus, it cannot be logical to aim to insert a needle intrathecally [i.e. through the dura] above the spinous process of L3." Research is being done on the advisability of using ultrasound to guide lumbar puncture.
In cases where there are signs of increased intracranial pressure (e.g., edema of the optic
disc, which is called papilledema), lumbar puncture must be performed with great care because it entails the risk
of a rapid drop in spinal fluid pressure, which would then result in a pressure differential between the fluid around
the brain and that around the spinal cord. This pressure differential may then push the brainstem
and cerebellar tonsils downward through the foramen magnum, causing death. If there are signs
of increased intracranial pressure, some physicians prefer to withdraw CSF from a site above the
foramen magnum. There is a substantial pool of CSF between the inferior surface cerebellum and
dorsal surface of the medulla. This pool is called the cisterna magna, and it can be approached by
a needle inserted upward and forward between the posterior arch of the atlas and the occipital
bone. Such a cisternal puncture should only be attempted by someone skilled in its practice, as
the risk to the brainstem is substantial.
Lumbar Epidural Anesthesia
In epidural anesthesia the anesthetic is injected into the epidural space. This entails essentially no risk of undesired spread of anesthetic to higher regions of the CNS (as can
occur if anesthetic is injected into the CSF), and it is compatible with insertion of a catheter that
allows continuous administration of anesthetic. It may be done at any level, but is particularly common in the lumbar region for control of labor pain. Entry of a needle into the epidural space does not place either the spinal cord or spinal rootlets at risk, but of course one can mistakenly push the needle too far.
The technique of lumbar epidural anesthesia is similar to that of lumbar puncture performed for another reason. While the preferred site of needle insertion is still the L3/L4 interspace, there is little reluctance (possibly not justified) in attempting to enter the L2/L3 interspace. The trick in an epidural block is to pierce the ligamentum flavum but stop
before you pierce the dura, thus ending up in the epidural space. This is often done by using the
air-rebound technique. The needle is attached to a syringe filled with air. When you are
superficial to the ligamentum flavum, any attempt to inject the air will meet with resistance and
the plunger of the needle will rebound. When you have entered the epidural space, there is a
negative pressure, and the air will be sucked in. You then exchange the air-filled syringe for one
with anesthetic, or you pass a catheter through the needle. Depending on the volume of anesthetic
injected, or the direction of the catheter, one can control how many spinal nerves are
anesthetized. Sacral Epidural Anesthesia (saddle block)
This is a method of anesthetizing sacral spinal nerves. It takes advantage of the fact that the
sleeve of spinal dura/arachnoid is shorter than the vertebral column. The dura and arachnoid end at S2. Thus, one may introduce anesthetic
into the relatively wide epidural space of the sacral vertebral canal via a needle inserted through
the sacral hiatus. This is called a saddle block because the area of skin anesthetized is pretty much what would be in contact with a saddle upon which one was seated. Saddle block was designed primarily for anesthetizing the perineum during
childbirth. It is no longer popular. One reason for its demise is because there is a tendency for fecal
matter to leak from the anus and contaminate the site of entry of the catheter. The other reason is
the great success of lumbar epidural block for obstetrics.
An approach to the epidural space
through the sacral hiatus is used by some physicians to inject anti-inflammatory drugs for the
treatment of spinal nerve compression caused by arthritic changes in the lumbar intervertebral
joints. The value of this treatment is not universally accepted. Breast
A superolateral extension of breast glandular tissue reaches into the axilla. It is called the axillary tail of
Spence. If cystic, it will present as palpable swellings in the armpit.
If breast cancer spreads to a Cooper's ligament, it will be shortened, causing a dimple in the skin of the breast. Clinical Sidelights on Lymphatic Drainage of the Breast
Aortic Coarctation
Coarctation of the aorta is a congenital narrowing of this vessel, usually along the aortic arch
just distal to the origin of the left subclavian artery. Consequently, a greatly reduced amount of
blood reaches the descending aorta from the arch. Alternate routes to the descending aorta become dilated, so that
enough blood reaches it and the lower part of the body is kept alive. As stated in
this chapter, one such alternate route exists by virtue of anastomoses between anterior and
posterior intercostal arteries. In a typical aortic coarctation, blood is still able to pass normally from the aortic arch into the
subclavian, internal thoracic (internal mammary), and anterior intercostal arteries on both sides. It then travels through anastomotic
channels into posterior intercostal arteries, and can continue "backward" in these vessels to reach
the descending aorta. Now, whenever arteries are subjected to a sustained increase in flow, they respond
by enlargement. (When flow is reduced in an artery for a sustained period, it responds by a
reduction in diameter.) In aortic coarctation, the intercostal arteries and the anastomotic channels
between them become greatly dilated. A pulse can then be felt in the intercostal spaces, and the
dilated tortuous intercostal arteries press on the inferior borders of the ribs, causing localized
areas of bone resorption that can be seen in Xrays as notching of the inferior borders of rib.
There are other anastomotic pathways that can bring blood from branches of the aortic arch
to the descending aorta. Two foremost among these are (1) the anastomosis between the epigastric arteries, and (2) anastomoses between arteries feeding muscles attaching to the scapula. You will be able to deduce the participants of the former as you learn more anatomy. The latter is
described in Core Concept 86. Posterolateral Thoracotomy
One approach to lung surgery is a standard posterolateral thoracotomy. A giant incision is
made transversely along the lateral aspect of the chest. The latissimus dorsi and serratus anterior
are both transected. After these big muscles are cut, the intercostal space is opened. Most
surgeons prefer to enter the fifth intercostal space because the major
fissure lies here, and through the major fissure one can gain ready access to the vessels of the hilum. During the surgery, you can
determine which interspace is the fifth by running your hand up alongside the chest wall deep to
the serratus anterior until to you feel the first rib, identifiable because it lies more "inside" the
second rib than above it. If you can't feel that high, your next best guide is that the interspace
between the second and third ribs is wider than the more inferior interspaces. As always, once you have identified the proper intercostal space, the
incision through intercostal muscles is made just superior to
the lower bounding rib, so as to avoid the intercostal neurovascular bundle. The surgeon should
pay particular attention to this requirement as the incision progresses posteriorly, because the
intercostal neurovascular bundle moves closer to the center of the intercostal space near the
vertebral column. It is unwise to extend the incision further medially
than the articulation of the rib with the transverse process of the vertebra. As the incision is
extended anteriorly, the surgeon must be certain to stop
short of the internal thoracic (internal mammary) vessels. NOTE: Newer techniques allow for a much smaller incision and less muscle cutting, so you may never see what I have described.
In the adult, a little pocket of parietal serous pericardium may bulge out through an acquired
defect in the fibrous pericardium to produce a so-called pericardial diverticulum. Although
uncommon and asymptomatic, pericardial diverticula do alter the cardiac shadow on Xray.
Inhaled Matter
As a result of the asymmetric position of the carina, inhaled foreign objects tend to pass into
the right mainstem bronchus, and thus into the right lung more frequently than into the left. If a person is supine (as during surgery), foreign material entering the bronchial tree (whether on the right or the left) will likely flow into the
posteriorly placed segments of the lung, most often the posterior segment of the upper lobe and the superior segment of the lower lobe.
Segmentectomy
While lacking the independence of lobes, bronchopulmonary segments are sufficiently
autonomous that infection, pneumonia, or atelectasis (collapse) may affect one segment while its
neighbors remain normal. It is even possible surgically to resect a single bronchopulmonary
segment. This is done by deflating the lung, tying off the bronchus and artery to the diseased
segment, re-inflating the lung, and then removing the tissue that is unfilled by air. Obviously, it is
the veins between segments that are at greatest risk during such surgery. Segmentectomies are
not common procedures. They are done only if it is of paramount importance to preserve as much
lung tissue as is possible. A segmentectomy might be done in a patient with a solitary pulmonary
cancer nodule who has poor pulmonary function, but in this case the surgeon might opt for a
wedge resection (i.e., taking out a wedge of tissue including and surrounding the tumor), which is nonanatomic.
A Bit of Detail About Autonomic Innervation of, and Sensation from, the Bronchi and Lungs
As you would expect, the smooth muscle of bronchial vasculature receives both sympathetic and parasympathetic innervation. Also, as is to be expected, the smooth muscle and glands of bronchi receive a rich parasympathetic innervation. What is surprising is that the smooth muscle and
glands of the bronchial tree receive little or no sympathetic innervation (Middleton's Allergy Principles & Practice, 6th Edition. 2003. N. Franklin Adkinson Jr et al., eds., Mosby, Phila.). To quote a recent review (Canning BJ, Fischer A. 2001 Neural regulation of airway smooth muscle tone. Resp Physiol 125:113-127), "The predominant contractile innervation of airway smooth muscle is parasympathetic and cholinergic in nature, while the primary relaxant innervation of the airways is comprised of noncholinergic (nitric oxide synthase- and vasoactive intestinal peptide-containing) parasympathetic nerves. ... Sympathetic-adrenergic nerves play little if any role in directly regulating smooth muscle tone in the human airways." This is seemingly due to a "paucity of adrenergic nerve fibers innervating the airway smooth muscle". I want to emphasize, however, that airway smooth muscle does relax in response to circulating adrenal medullary hormones.
The lung does not experience pain. It is true that visceral afferent fibers run alongside vagal autonomic fibers, but these afferents do not carry pain sensu stricto. They carry information on stretch (which, however, does not seem to
reach consciousness), and they probably carry the sense of discomfort that one experiences after
mechanical or chemical irritation, or during asthmatic attacks. Origins of Coronary Arteries from the Sinuses of the Aortic Valve
This sidelight arose when I discovered my own misunderstanding of a basic anatomical fact. I have a friend with narrowing of the aortic valve (aortic stenosis) due to calcification of its cusps. The resulting loss of cusp flexibility means they cannot move away from one another sufficiently to create an adequate opening for blood to pass out of the heart into the ascending aorta. My friend told me he would be undergoing valve replacement by a procedure called Transcatheter Aortic Valve Replacement (TAVR) that is done without open heart surgery. (You can see a nice desciption of aortic stenosis and TAVR on YouTube.) He said the procedure did not entail removing the diseased cusps. Rather, these cusps would be pushed against the inner wall of the aorta to make room for the prosthetic valve. I was incredulous, thinking that cusps pushed up against the aortic wall would block the openings (ostia) of the coronary arteries arising from the walls of the valvular sinuses. It turns out that my incredulity was based on a false notion that the coronary ostia lie near the middle of the valvular sinuses. In truth, they are located near the upper limit of the sinuses, and in most people will be above the upper edge of the cusps
(Knight J, et al. 2009 Ex vivo and in vivo coronary ostia locations in humans. Surg Radiol Anat 31:597-604; He Z-F et al. 2014 In vitro study of coronary flow occlusion in transcatheter aortic valve implantation. J Thorac Dis 6:1772-1777) .
Coronary Dominance
As stated in the chapter, coronary dominance is defined by the vessel that gives rise to the
posterior descending artery. While coronary angiographers routinely report which vessel is
dominant, it is not so obvious how this information is clinically useful. There is one report that
individuals undergoing bypass surgery for left main coronary artery stenosis have a higher
perioperative mortality if they are left coronary dominant. Also, in left dominant hearts the circumflex coronary artery
lies closer to the rim (anulus) of the mitral valve (maybe because the
vessel is bigger), and as a consequence is more likely to be caught in a suture during mitral valve replacement surgery than
if the heart were right coronary dominant.
Course of the Posterior Descending Artery in a Right
Coronary Dominant Heart
A common variation is an early origin of the posterior descending artery from the right coronary
artery. In this case, the PDA comes off on the back surface of the heart prior to the junction of the
coronary sulcus with the posterior interventricular groove (which intersection is called the crux of the heart. Then, the PDA then just meanders toward the
posterior interventricular sulcus. The surgeon must be aware of this possibility if it is necessary
to bypass a block in the PDA.
Cardioplegia
Most coronary bypass and open-heart surgeries entail perfusion of the heart with cardioplegic solution - stuff that causes your heart to stop. In roughly half such cases, the cardioplegic solution is pumped backward in the coronary sinus to reach the capillary bed of the heart. This is called retrograde cardioplegia. (I hope you know that normal venous flow in the coronary sinus is away from the capillary bed, as is the case for veins in general.) Retrograde cardioplegia may be the sole means of introducing heart-stopping solution, or it may be combined with solution being sent through the left and right coronary arteries, which is called anterograde cardioplegia. In retrograde cardioplegia, the solution leaves the capillary bed via Thebesian veins, which are tiny veins that run from
heart capillaries directly into the cavities of all the heart chambers. Retrograde cardioplegia is only possible because of the existence of Thebesian veins, which present an alternate route of exit from the capillary bed.
False Heart Attack
Because the spinal cord segments receiving pain from the heart are the same as those
receiving pain from the thoracic esophagus, pain emanating from disease of the latter may be
confused with a heart attack. Maybe that's why 30% of persons who present with anginal pain
have normal coronary arteries (Garrison, DW et al., Pain 49:373-382).
An Uncommon Treatment for Cardiac Angina
For a variety of reasons, certain patients with intractable angina are not good candidates for coronary artery bypass grafts or coronary angioplasty. Because the pain arising from ischemia of the heart courses
along axons that follow the reverse route of sympathetic outflow to the heart, one method used to
treat these patients is to excise a portion of the upper thoracic sympathetic trunk from the T2 - T5 ganglia inclusive. This has been shown to reduce the number of anginal episodes in the course of the patient's daily activities. The surgery has the additional effect of increasing the time the patient can engage in formal exercise before experiencing anginal pain. Maybe there is reduced myocardial oxygen demand
during exercise because of a secondary effect of the sympathectomy to reduce heart rate and
blood pressure during exercise (Wettervik, C et al. 1995 in The Lancet 345:97-98).
The
top of spinal cord segment T1 lies opposite top of vertebra T1.
The top of
spinal cord segment L1 lies opposite top of vertebra T11.
The top of
spinal cord segment S1 lies opposite top of vertebra L1.

Of course, there is individual variation and the precise location of the ostia in your patient should be determined by angiography before embarking on a TAVR.
During surgery in the superior mediastinum, it is possible to mistakenly nick one of the pulmonary arteries. In order to temporarily control bleeding, it is far easier to open the pericardium and clamp the pulmonary
trunk within the pericardial sac than to try to clamp the damaged vessel in the superior
mediastinum.
Left Recurrent Laryngeal Nerve
In the chest, the left recurrent laryngeal nerve is subject to compression by aortic arch aneurysm, pulmonary trunk dilation (as can occur if the mitral valve is stenotic, leading to pulmonary hypertension), tumor of the esophagus, or tumor in tracheal lymph nodes. Thus, hoarseness (a symptom of recurrent laryngeal nerve dysfunction - see Core Concept 74) may arise from thoracic disease. The nerve may be damaged during surgery in the superior mediastinum, particularly for treating trauma to the aortic arch.
Broncho-aortic Constriction of Esophagus
The site where the esophagus is crossed on its left side by the aortic arch and, below this, where the esophagus is crossed anteriorly by the left mainstem bronchus, is the so-called broncho-aortic constriction. It can be visualized on barium swallow and is one of the more common sites of esophageal cancer.
Left Atrial Hypertrophy and the Esophagus
If the left atrium is enlarged, as in mitral valve disease, it will displace the esophagus posteriorly. This is easily recognized on Xrays of a barium swallow. In the days before CT, taking a lateral chest Xray during a barium swallow was considered an excellent way of identifying left atrial hypertrophy. It still is a cost-effective way, and is used if CT equipment is not available.
Phrenic Nerves and Diaphragm Paralysis
A lot of attention is paid to the location of the phrenic nerves in the chest because one wants to avoid injury to them during chest surgery. Nonetheless, such injury does occur, more usually to the left phrenic nerve than the right. Major damage to the phrenic nerve produces paralysis of the ipsilateral hemidiaphragm. (There are a other causes of unilateral diaphragm paralysis, but surgical trauma is among the top four or five.) Interestingly the majority of patients with unilateral diaphragm paralysis are asymptomatic in normal daily activities, although their arterial O2 concentration is lower than normal and they cannot sustain exercise as long as a normal person. About a quarter of such patients have shortness of breath upon exertion (exertional dyspnea) and when lying down (orthopnea). The biggest problem with unilateral diaphragm paralysis is atelectasis (i.e., collapse) of the ipsilateral lung. Chronically atelectatic lungs are predisposed to get pneumonia. Hence, the treatment for unilateral diaphragm paralysis is surgical plication of the paralyzed hemidiaphragm, a procedure in which that hemidiaphragm is shortened by folding it over on itself and suturing the folds together. The affected lung then expands to fill the enlarged pleural space and is less likely to become pneumonic. This procedure also helps with symptoms, if present.
Bilateral diaphragm paralysis is less common than unilateral paralysis and generally results from a nervous system disease that widely affects muscles (e.g. ALS). In and of itself, bilateral diaphragm paralysis is not fatal. Severe exertional dyspnea and orthopnea are pretty constant symptoms. The latter problem is treated with positive pressure ventilation during sleep. Bilateral plication of the diaphragm may be attempted.
Size of the Heart
A heart whose apex is lateral to the mammary line is clearly enlarged or displaced.
Heart Sounds
The sounds created by cardiac valves are best heard along the path of blood that has passed
through the valve, i.e., just distal to the valve itself. From a knowledge of valve position one may
deduce the following as good sites:
Tricuspid Valve - texts on physical diagnosis differ; some say to listen directly above the xiphisternal joint, others say to place the stethoscope at the medial Mitral Valve - over
the apex of the heart.
Pulmonary Valve -
at the medial end of left 2nd intercostal space .
Aortic Valve - at
the medial end of right 2nd intercostal space.
end of the left 5th intercostal space.
Pericardiocentesis
The most important reasons for knowing the surface projections of the pleural cavities have
to do with choosing sites to introduce a needle for the purpose of withdrawing excess pericardial fluid
or excess pleural fluid.
Withdrawing pericardial fluid (or blood, or pus) is called pericardiocentesis. A prime objective is to avoid
penetrating the lung. It is also important that one not stick a needle through the internal thoracic (internal mammary) artery. One would like to avoid the left pleural sac, though this is a less crucial requirement. Current recommendations are that pericardiocentesis be done under ultrasound guidance, especially if there is no emergency. The patient is often placed in a position that causes pericardial content to flow inferiorly and to the left. Ultrasound reveals where the accumulation is greatest, and where it is closest to the body surface. Often it turns out that the best site for inserting the needle is in the fifth intercostal space a variable distance lateral to the internal thoracic artery. Since ultrasound does not go through air, you are pretty much guaranteed that any fluid you can visualize is not covered by lung. Obviously, when inserting the needle, you stay close to the superior surface of the lower bounding rib so as to avoid the intercostal neurovascular bundle.
In an emergency, when there is so much fluid or blood in the pericardial space that the resulting pressure on the heart prevents it from filling adequately during diastole (a condition called cardiac tamponade), you might have to do a "blind" pericardiocentesis. The preferred method is a left substernal paraxiphoid approach, usually called the subxiphoid approach. A needle is inserted in the angle formed by the left border of the xiphoid process and the 7th costal cartilage. The needle is angled 45° to the skin and directed toward the midpoint of the left clavicle, or toward the left shoulder. If all goes well, the needle will pass anterior to the diaphragm's origin from the xiphoid process and ribs. Nonetheless, there is the risk that the needle will go below the diaphragm and injure the liver.
A old method of pericardiocentesis is the left parasternal approach. The needle was inserted through the left 5th intercostal space immediately adjacent to the sternum (thereby medial to the internal thoracic artery and likely to miss not only the lung but also the pleural sac). This approach fell out of favor because of a higher risk of damaging the LAD, although I imagine this risk is less if the amount of pericardial fluid is great.
Thoracentesis
Withdrawal of excess fluid from the pleural cavity is called thoracentesis. The fluid tends to collect posteriorly and laterally in the most dependent portions of the pleural cavity. Logic might suggest that one try to insert the needle into the costodiaphragmatic recess as close to the lower limit of the pleural cavity as possible. This would be a mistake. Even in cases of pleural effusion the costodiaphragmatic recess is not very wide, because the pressure of the abdominal organs pushes the periphery of the diaphragm toward the inner surface of the rib cage and keeps the costodiaphragmatic recess narrow. Inserting a needle too close to the lower limit of the pleural cavity runs the risk of passing through the recess and diaphragm into the abdominal cavity. The general rule is that potential sites of insertion inferior to the 9th rib are to be avoided. (Indeed, needle biopsy of the liver is often done by inserting the needle through the 9th intercostal space in the right midaxillary line, with full knowledge that it will pass through the costodiaphragmatic recess and diaphragm to reach the liver. In accessing the liver this way, the patient is asked to hold expiration so as to minimize any chance of piercing the lung.) The most usual site of thoracentesis is just below the inferior angle of the scapula with the arm abducted 90 degrees. This corresponds to the 6th or 7th interspace near the posterior axillary line. Other routes may be chosen depending on radiologic findings.
Auscultation of the Lung (Listening to the Lung with a Stethoscope)
You can predict what part of a lung will be heard with a stethoscope if you know the surface
projections of the lobes and the position within a lobe of the bronchopulmonary segments.
It is most important to realize that you cannot hear the lower lobe along the front of the
chest, and you cannot hear the middle lobe in the midaxillary line.
(1) A
stethoscope placed in the supraclavicular fossa (i.e., just superior to medial third of the clavicle)
will hear the apical segment of upper lobe.
(2) A stethoscope placed on the back not far from the
vertebral column will hear (a) the posterior segment of the upper lobe if the stethoscope is placed superior to the site where the spine of the scapula meets its vertebral border; (b) the superior segment of the lower lobe if the stethoscope is placed just
inferior to the site where the spine of the scapula spine meets its vertebral border; (c) the posterior basal segment of the lower lobe if the stethoscope is placed
medial to the inferior angle of the scapula. (3) A
stethoscope placed in the midaxillary line will hear (a) the upper
lobe if the stethoscope is placed above the 5th rib; (b) the lower
lobe (lateral basal segment) if the stethoscope is placed from the 5th to 8th ribs. (4) A
stethoscope placed on the front of the chest between the midclavicular line and the sternum will
hear (a) the upper lobe (anterior segment) if the stethoscope is placed
above the 4th costal cartilage (b) on
the right side, the middle lobe (medial segment) if the stethoscope is placed from the 4th to 6th costal cartilages.
Lumbocostal Trigone
For developmental reasons, the part of the diaphragm arising from the lateral arcuate ligament (on the surface of quadratus lumborum) and from the 12th rib may be deficient in actual muscle tissue (i.e., represented only by epimysium). The deficient region is said to comprise a lumbocostal trigone and is a potential site of herniation of abdominal contents into the thoracic cavity. The herniated structures will be covered by stretched epimysium.
Transversus Abdominis Plane (TAP) Block (I wish to acknowledge my colleague Nathan Kley for drawing my attention to the existence of TAP block.)
For parts of their courses the 7th - 11th intercostal nn., subcostal n., iliohypogastric n., and ilioinguinal n. all travel toward the front of the body by running in the plane of tissue between the transversus abdominis and internal abdominal oblique. In recent years in has become popular to inject local anesthetic into this plane in order to lessen the postoperative pain following either laparoscopic or open abdominal surgery. If the goal is to anesthetize the anterolateral abdominal wall from T10 inferiorly, the needle is inserted at the midaxillary line between the costal margin and the iliac crest. For anesthesia of the abdominal wall served by T7 - T10, a more anterior and superior subcostal injection site is chosen. Ultrasound is used to determine the correct intermuscular plane and to follow the needle as it is being inserted. I cannot describe the procedure nearly as well as can be shown by films available on YouTube. I suggest you start with https://www.youtube.com/watch?v=9TIHDn7uBZI. For a better close-up view of the injection try https://www.youtube.com/watch?v=CzMDdrPbLEM, and for a brief discussion of the subcostal approach look at the first three minutes of https://www.youtube.com/watch?v=9iXkZ8KG2X4.
Superficial Epigastric Artery
After arising from the common femoral artery, the superficial
epigastric artery enters the subcutaneous layer and runs upward in Camper's fascia. This path
crosses that of the incision (running from anterior superior iliac spine to the pubic tubercle) that
is made during an external repair of an inguinal
hernia. (An external repair is one made from the outside, as opposed to a laparoscopic repair, which is made from inside the abdominal cavity.) During external repair of an inguinal hernia, the surgeon must identify and tie off the superficial epigastric artery, or else the patient
will develop a bad hematoma.
Sympathetic innervation of the testis derives from T12-L1 of the spinal cord. As predicted, visceral sensory axons from the testis travel "backward" alongside the sympathetic axons to reach the T12-L1 segments of the spinal cord. Testicular pain
is referred to the T12-L1 body wall segments, predominantly along the distribution paths of the
iliohypogastric and ilioinguinal nerves.
Clinical Nomenclature
Clinicians often use different names for inguinal structures than do anatomists (although this
is becoming less frequent). The inguinal ligament may be called Poupart's ligament; the lacunar
ligament may be called Gimbernat's ligament. I don't like these eponyms, but sometimes I do
prefer clinical terminology. For example, I prefer to use the term Cooper's ligament for the
thickened periosteum behind the pecten pubis (see Core Concept 94), whereas less ecumenical
anatomists call it the pectineal ligament.
Clinicians also define a space called Hesselbach's triangle. It is bounded by the inguinal
ligament (inferolaterally), the lateral edge of the rectus abdominis (medially), and the path of the
inferior epigastric artery (superolaterally). Direct inguinal hernias begin their push through the abdominal
wall in the region of Hesselbach's triangle. In that indirect inguinal hernias start at the deep inguinal ring, their path begins lateral to Hesselbach's triangle.
More About Direct Inguinal Hernias
Clinical texts describe a variety of ways in which direct inguinal hernias may present
differently from indirect hernias. First, in males direct hernias are less likely to pass into the
scrotum than are indirect hernias. A further difference can be deduced from the knowledge that
only indirect hernias pass through the deep ring. Often when a patient lies on his or her back, the
herniated structures fall back into the abdominal cavity. They can be made to herniate again if the
patient strains. In the case of small indirect hernias, this voluntary reherniation can be prevented
by the examiner pressing his or her thumb over the site of the deep ring (near the midinguinal point).
Such pressure will have no effect on preventing reherniation of direct hernias. Although this maneuver is often recommended as a way that a physician may differentiate indirect from direct inguinal hernias by physical examination, several studies report that in actual practice it is so unreliable as to be not worth the effort (Sanjay P et al.. 2010 Anatomical differentiation of direct and indirect inguinal hernias: is it worthwhile in the modern era? Clin Anat 23:848-850). One source of the problem may be variability in deep ring position.
Frequency of Hernias
As stated in the chapter, the frequencies of indirect inguinal
hernias, direct inguinal hernias, and femoral hernias are highly dependent on sex and age. This
topic has been reviewed by Rutkow (Surg. Clinics North Amer., 78:941-951, 1998). While
statistics vary from study to study, the following table is not far off the mark in presenting the
expected distribution of 100 hernias of the groin by sex.
| Inguinal | Femoral | |||
|---|---|---|---|---|
| MALES | 58 | indirect | ||
| 29 | direct | |||
| 87 | total | 2 | ||
| FEMALES | 6.6 | indirect | ||
| 0.4 | direct | |||
| 7 | total | 4 |
Not reflected in these
numbers
is the fact that the ratio of indirect to direct inguinal hernias in males is greatly influenced by age, there
being a much higher proportion of indirect inguinal hernias in young boys because (a) so many
inguinal hernias in young males are due to partial persistence of the processus vaginalis, and (2) as
one becomes older, musculofascial weakness predisposes to direct inguinal hernias.
Canal of Nuck
In female fetuses there develops a small processus vaginalis that extends through the inguinal canal alongside the round ligament. This small processus vaginalis goes by the name "canal of Nuck". Almost always it obliterates before birth. Rarely it stays patent, and very rarely, if its communication with the peritoneal cavity becomes narrowed or obliterated, may accumulate enough fluid so that it presents as a swelling in the groin. This is called a hydrocele of the canal of Nuck and may occur at any age. Some authors believe that indirect inguinal hernias in females can be traced to the persistence of the canal of Nuck. This is almost certainly the case for congenital indirect inguinal hernias in girls, but these are also very rare.
Hepatic Blood Supply
The liver receives blood from two sources: the common hepatic artery and the portal vein.
Because the volume of flow through the portal vein is so much greater than that through the
hepatic artery, some texts say that 50-55% of the liver's oxygen is actually provided by the
venous route even though venous blood is of much lower oxygen concentration. A
physiologically healthy liver with normal portal venous flow should survive inadvertent right or
left hepatic artery ligation. For example, if you tie off the right hepatic artery, although the
patient will experience an ischemic hepatitis (with pain and the release of liver enzymes into the
blood), 80% of people will recover from this condition. Intrahepatic collateral circulation
between the right and left hepatic arteries contributes to the long-term survival of a liver
lobe whose artery has been ligated (Mays ET, Wheeler, CS 1974 Demonstration of collateral arterial
flow after interruption of hepatic arteries in man. N Engl J Med 290:993-996).
Surgical Nomenclature for Liver Lobes
As stated in Core Concept 24, the right branches of the portal vein and hepatic artery
distribute to the right lobe of the liver, whereas the left branches of these vessels go the caudate,
quadrate, and left lobes (in truth, the caudate often gets supplied by both the right and left branches
of the portal vein and hepatic artery). The right hepatic bile duct drains the right lobe of the liver;
the left duct drains the other three lobes (but again, the caudate lobe often drains to both right and left hepatic ducts). Surgeons recognize the physiological division of the
liver by using the term "left lobe" to include the caudate and quadrate lobes along with the
anatomist's left lobe. The plane between the physiological right
and
left lobes is coincident with a line drawn from the middle of the cystic fossa to the left edge of
the caval fossa. This is called Cantlie's line.
Hepatic Veins
There are three major hepatic veins that enter the IVC. They are called right, middle and left. The middle vein lies deep within the liver along Cantlie's line, hence at the boundary between the physiological left and right lobes. It receives tributaries from both lobes. The middle and left hepatic veins usually join before entering the IVC. There are also a variable number of short hepatic veins (on average less than 3 mm in diameter) passing from the region of the liver surrounding the caval fossa directly into the IVC. These small hepatic veins must not be overlooked when removing parts of the liver in the vicinity of the caval fossa (see below). From a surgical point of view, it worth noting that there is a narrow zone running supero-inferiorly along the anterior surface of the IVC that receives no hepatic veins.
Liver Segmentation, Hepatic Lobectomy, and Hepatic Segmentectomy
Surgeons place emphasis on the fact that the lobes of the liver can be further
divided into segments based on the distribution of secondary and tertiary branches of the vascular
and biliary trees. (You will recall that a similar segmentation occurs in the lung.) Some
classifications refer to four major hepatic segments:
If the patient has a tumor nodule confined to
one segment of the liver, that segment alone may be removed. However, the most common types
of partial liver resections are To perform a hepatic lobectomy, the surgeon goes to the porta hepatis and ties off the artery,
vein, and bile duct of the portal triad going to the relevant lobe. The part of the liver that turns gray is
then resected. In cases of right lobectomy, the boundary between the red and gray parts will be
Cantlie's line; the middle hepatic vein lies in this
boundary and must be preserved, though its tributaries from the right lobe must be ligated. The right hepatic vein is tied off as it enters the IVC, as are any short hepatic veins passing from the right lobe to the IVC.
One of the dangers of a left lateral segmentectomy is due to the
fact that deep to the fissure of the ligamentum teres (which surgeons call the umbilical fissure)
lies the only branch of the portal vein that does not follow arteries and bile ducts. This
"umbilical" part of the portal vein gives branches to both the left medial and left lateral segments.
During a left lateral segmentectomy this umbilical part of the portal vein must be preserved; only
its branches to the left lateral segment are tied off.
A method of hepatic resection that requires less knowledge of anatomy is the wedge
resection. The surgeon just places clamps between the tumor-bearing part of the liver and the
good part, then cuts out the former, clipping vessels and bile ducts along the way. Gallbladder Pain
Most pain fibers from the gallbladder travel centrally in the same nerve bundles that bring
sympathetic innervation to that structure. Since the foregut receives its sympathetic innervation
from T5-T9, and the gallbladder is an outgrowth from the distal end of the foregut, you would be
correct to deduce that its pain fibers mainly return to T7 - T9 segments of the spinal cord.
Referred pain of cholecystitis or gallstones is usually felt along the right 7th - 9th intercostal
spaces, sweeping from back to front near the inferior angle of the scapula toward the epigastric
region.
Pain from the gallbladder may be referred to the right shoulder (C3,4). Some people believe
this is due to irritation of the peritoneum on the
undersurface of the diaphragm, which is innervated by the phrenic nerve (C3,4,5). I have also
read that the phrenic nerve, after it has pierced the
diaphragm to innervate that muscle's undersurface, gives a sensory twig that eventually reaches
the gallbladder. Cholecystectomy
During cholecystectomy, if the surgeon identifies a cystic artery that seems to be too large, it
should be dissected out to make certain it is not a hepatic artery. If the cystic artery seems to
small, consideration must be given to the possibility that it is only an anterior branch of the cystic
artery, or that the patient has an anomalous double cystic artery. If the surgeon ties off only the
anterior branch, or only one of two cystic arteries, believing that it is the entire and only vessel,
there will be lots of bleeding when the gallbladder is pulled out.
A common anomaly of the biliary system is the existence of a small bile duct that leaves the
right lobe of the liver and runs in the gallbladder bed (i.e., in the subvesicular connective tissue
between the gallbladder and the liver) to reach the right hepatic or common hepatic bile duct.
This "duct of Luschka" can be injured in cholecystectomy. Also, there may be tiny bile ductuli
that leave the liver substance to end blindly in the subvesicular connective tissue. These are a
source of self-limiting bile leakage following a cholecystectomy.
A more detailed classification divides each of these four
segments into two, creating eight segments in total.
1) left lateral segment, which is the
anatomist's left lobe
2) left medial segment, which
comprises the anatomist's quadrate and caudate lobes
3) right anterior segment, the anterior
part of the right lobe
4) right posterior segment, the posterior
part of the right lobe.
1) right lobectomy - removal of both
major segments of the right lobe
2) left lobectomy - removal of the left
medial and left lateral segments (i.e., caudate lobe, quadrate lobe, and the anatomist's left
lobe)
3) left lateral segmentectomy - removal
of the anatomist's left lobe
4) right trisegmentectomy - removal of
the right lobe (which has two major segments) and the left medial segment (caudate and quadrate
lobes)
Identifying Bowel Segments at Surgery
Upon entering the peritoneal cavity via an anterior abdominal incision, any mesenteric
portion of the bowel may be encountered first. Thus, the surgeon is confronted with deciding
whether a particular loop of bowel might be jejunum, ileum, transverse colon, or sigmoid colon.
First, decide if it is colon by looking for appendices epiploicae and taenia coli. If it is colon,
decide if it is transverse or sigmoid using the following criteria: (a) transverse colon is attached
to three mesenteries (gastrocolic ligament, apron of greater omentum, and transverse mesocolon),
whereas sigmoid colon is attached only to its mesocolon, and (b) transverse colon (like ascending
and descending colons) has three taenia coli, whereas the sigmoid colon has only two.
If you have determined that the loop of bowel isn't colon, decide if its jejunum or ileum using
the following criteria: (a) mesenteric fat does not uniformly reach the wall of the jejunum, whereas mesenteric fat
overlaps the wall of the ileum, and (b) the arterial supply to the jejunum is characterized by 1 or 2
arcades with long vasa recta (Core Concept 26), whereas the arteries to the ileum form 3 or 4 arcades
with short vasa recta.
The Amazing Bloodless Fold of Treves
I help teach a surgical anatomy course to fourth-year medical students. During that course, a colleague (Dr. Fidel Valea) made mention of a structure with which I was completely
unfamiliar. It is called the "bloodless fold of Treves". I quote from Morris' Human
Anatomy (pp. 1379-1380, 11th edition, eds. J. P. Schaeffer et al., McGraw-Hill,
NY):
"If the appendix is drawn caudally so as to put its mesentery on the
stretch, a peculiar fold will be found to join that mesentery. This
inferior ileocecal fold arises from the border of the ileum opposite the
attachment of the mesentery. It then passes across the ileocecal
junction on its caudal aspect and is adherent to the cecum., and finally
joins the surface of the mesentery of the appendix. This fold is
peculiar in that it scarcely has any visible vessels, and is often known
as the 'bloodless fold of Treves'."
Sir Frederick Treves, who first described this structure, is nowadays more noted for having
treated the "Elephant Man". I am told by Matthew Ranzer (a former medical student at Stony Brook) that
Treves was also well known for having performed an appendectomy on Edward VII, King of
England. According to Ranzer, the king desperately needed an appendicitis operation but
strongly opposed going into a hospital. 'I have a coronation on hand,' he protested. But Treves
was adamant: 'It will be a funeral, if you don't have the operation.' Treves won; the coronation
was postponed and the king lived.
In Treves' own textbook of anatomy he does not describe the significance of the bloodless
fold that now bears his name. Dr. Valea states that "it is, at times, a useful landmark, when you
have limited exposure, to identify the terminal ileum as it is the only place
on the small bowel that has antimesenteric fat." Another of my colleagues (Dr. Joseph Sorrento)
says it can help him locate the appendix. Personally, I find its history as
interesting as its clinical significance. Location of the Splenic (Left Colic) Flexure
The transition between the transverse colon and the descending colon is properly called the left colic flexure. Every book I have ever seen, including Core Concepts, says it is located adjacent to the inferior pole of the spleen. Hence, this bend in the colon is commonly called the splenic flexure. In reviewing CTs of the abdomen while preparing to deliver a lecture on radiology, I kept on coming across normal people in whom the junction of the transverse colon with the descending colon was located just below the diaphragm, not at the inferior pole of the spleen. You can see an example for yourself by looking frame-by-frame at a video I created from a series of relevant coronally reformatted CT slices. The frames proceed from posterior to anterior. When I questioned some surgeons, they confirmed that although the "splenic flexure" of the colon is near the spleen, it is not always up against its inferior pole.
Pain
Derivatives of the midgut receive sympathetic innervation from T9-T12. The appendix is
innervated predominantly by T10. Referred pain from appendicitis is located in the T10 body
wall segment, thus in the vicinity of the umbilicus. When there is additional somatic pain located
in the abdominal wall over the appendix, this indicates spread of inflammation to the nearby
parietal peritoneum.
McBurney's Point
In 1889 the American surgeon Charles McBurney made the following observation:
"Whatever may be the position of the healthy appendix found in the dead-house, and I am well
aware that its position when uninflamed varies greatly, I have found in all of my operations that it
lay, either thickened, shortened, or adherent, very close to its point of attachment to the caecum.
This, of course, must, in early stages of the disease, determine the seat of greatest pain on
pressure. And I believe that in every case the seat of greatest pain, determined by the
pressure of one finger, has been very exactly between an inch and a half and two inches from
the anterior spinous process of the ilium on a straight line drawn from that process to the
umbilicus." (McBurney C 1889 Experience with early operative interference in cases of disease
of the vermiform appendix. New York Med Jour 50:676-684.)
Nowadays, McBurney's Point (of maximal tenderness in acute appendicitis) is said to be at the
junction of the lateral one-third and middle one-third of the line between the anterior superior iliac spine
and the umbilicus. Whereas McBurney thought this corresponded to the base of the appendix,
recent studies suggest that the latter is usually inferomedial to McBurney's point. Nonetheless,
physicians still consider maximal tenderness at McBurney's point to be a strong indicator of acute
appendicitis. White Line of Toldt
You will recall that in embryonic development the ascending colon "falls" to the right side and becomes secondarily retroperitoneal. Its mesentery, which carries its vascular supply, fuses with the parietal peritoneum medial to the ascending colon. After this happens, along the right edge of the ascending colon is the zone where the peritoneum on its anterior surface merges with the parietal peritoneum lateral to it. This is a relatively avascular zone of peritoneum. Similarly, in embryonic life the descending colon "falls" to the left side, where it becomes retroperitoneal. Its mesentery, carrying its vascular supply, fuses with the parietal peritoneum medial to the descending colon. After this happens, along the left edge of the descending colon is the zone where the peritoneum on its anterior surface merges with the parietal peritoneum lateral to it. This too is a relatively avascular zone of peritoneum. These two zones of relative avascular peritoneum, one along the right edge of the ascending colon, the other along the left edge of the descending colon, are called the "white lines of Toldt". An incision is made along the respective white line of Toldt when either the ascending or descending colon needs to be mobilized for the purpose of removing it, or for gaining access to the ipsilateral kidney or ureter.
By the way, the regions of the peritoneal cavity on either sides of the white lines of Toldt (i.e., to the right of the ascending colon and to the left of the descending colon) are called paracolic gutters. Cancers that shed into the peritoneal cavity, such as ovarian or colorectal cancer, may seed the paracolic gutters, so the surgeon must look there (as well as behind the liver and spleen) when assessing for intraperitoneal metastases.
Portosystemic Venous Anastomoses
There is a fourth portosystemic anastomosis not mentioned in Core Concept 27. It occurs between
secondarily retroperitoneal mesenteric veins and the primarily retroperitoneal veins of the
posterior abdominal wall. Dilation of these anastomoses in portal hypertension is neither
observable nor symptomatic. The importance of these anastomoses is not related to portal hypertension, but to the fact that their existence provides routes for spread of bowel cancer to posterior body wall structures, including the vertebral column.
As stated in the chapter, bleeding from ruptured esophageal varices is the most serious
consequence of portal hypertension. Of those persons with cirrhosis of the
liver who actually experience esophageal variceal bleeds, 40% - 50% will die from their first bleeding episode
within six weeks. There are nonsurgical methods of treating esophageal varices, most notably
sclerotherapy, in which fiberoptic endoscopy is used to guide injection of a
thrombosis-promoting solution into the dilated veins.
The surgical method to relieve the portal hypertension is via a shunt between the portal venous network and
the systemic (nonportal) veins. The preferred method of creating a portosystemic shunt used to be via a surgical
connection of the portal vein to the inferior vena cava (i.e., a portacaval shunt). From an anatomic perspective, it's logical that a portacaval shunt would be the procedure of choice, because the portal vein and IVC are so close to one another at the epiploic foramen and, as a consequence, relatively easy to connect. It fell into disfavor because metabolic problems were caused by
diverting so much blood from the liver. Since the main goal of treating portal hypertension is to
eliminate the threat to life posed by esophageal varices, the currently preferred surgical procedure
is the splenorenal shunt, which consists of severing the splenic vein from its entry into the portal
vein and anastomosing it end-to-side to the left renal vein. You will recall that these two vessels
are in close proximity - the splenic vein lying on the posterior surface of the body of the pancreas
and the left renal vein being posterior to the lower border of the pancreatic body. At the same
time, the left gastric and right gastroepiploic veins are usually tied off so as to eliminate pathways
of venous return from the stomach that could circumvent the splenic vein.
There is also a new shunt technique that avoids abdominal surgery altogether. This entails
inserting a tubular device into the right internal jugular vein and threading it down the right
brachiocephalic vein, the superior vena cava, right atrium, and inferior vena into a large hepatic vein.
The device is then pushed through the wall of that hepatic vein into actual liver tissue, and through the liver tissue into one of the large branches of the portal vein. The tube now connects a large portal venous branch to a large hepatic vein. It is left in place to create an intrahepatic portosytemic shunt. The procedure is called Transjugular Intrahepatic
Portosystemic Shunt (TIPS) and is performed under radiologic monitoring. The problem with TIPS is
that the shunt tends to become blocked over time. It may be the method of choice if the patient
will soon have a liver transplant, because TIPS doesn't leave intra-abdominal adhesions that can
complicate the transplant surgery.
Anorectal varices caused by portal hypertension are more common if the portal hypertension has arisen from
obstruction of the portal vein outside the liver than from any hepatic disease, including cirrhosis.
In either case, bleeding is an uncommon occurrence, but such bleeding may be serious if the portal hypertension was caused by cirrhosis, because that disease is often associated with a defect in blood clotting.
Hemorrhoids are distinct from anorectal varices. To understand
this, one needs to know a little bit of detail about anatomy of the anal canal. For two centimeters
above the anus the inner lining of the anal canal is composed of a modified squamous epidermis
devoid of hair and glands. This is sometimes called anoderm. Above this region the inner
lining of the anal canal is composed of columnar epithelium, like the rest of the rectum. The line
of demarcation between anoderm and columnar epithelium is called the dentate or pectinate line. Below
the dentate line the anal canal is highly sensitive, as is regular skin; above the dentate line the
innervation is visceral in nature.
Both the anoderm and columnar epithelium rest upon a layer of submucosal tissue. Normally there are regions of dilated veins in the submucosa. If the submucosa, with its normal venous dilatations, becomes "loosened" from
deeper tissues and bulges into the lumen of the anal canal, this is a hemorrhoid (or pile). Sometimes the hemorrhoidal tissues prolapse downward
through the anus.
Hemorrhoids may originate below the dentate line - an external
hemorrhoid, above the dentate line - an internal hemorrhoid, or both. Because the covering of an
internal hemorrhoid is insensitive to somatic pain, it may be treated by ligation with a rubber
band.
The incidence of hemorrhoids in patients with portal hypertension is the same as in the
general population, illustrating the distinct nature of hemorrhoids from anorectal varices. The
latter can be distinguished from hemorrhoids because the venous swelling of a varix collapses
when pressure is applied and reappears rapidly when the pressure is released.
During surgery, celiac lymph nodes can be palpated for detecting spread of cancer. This is done by poking one's
finger through the hepatogastric ligament. To palpate more widely in the floor of the lesser sac,
surgeons poke their fingers through the gastrocolic ligament.
Accessory Renal Arteries
Knowing that accessory renal arteries are pretty common is important in renal transplant surgery. All arteries feeding the donor kidney must be linked together so that all will be fed when joined to an artery of the person receiving the transplant.
Renal Cell Carcinoma
Because the right renal vein is so short, renal cell carcinoma of the right kidney may readily enter the IVC and travel toward the heart. This tumor can usually be stripped out of the IVC because it does not adhere to its wall, but if the tumor does reach the heart, cardiac bypass is necessary to get it out.
Blood Supply to the Ureter
A ureter receives blood supply from several sources: a small twig from the renal artery, twigs
from the aorta and gonadal arteries, and small twigs from the internal iliac artery (and its branches, notably the
uterine in women and inferior vesical in men). Arterial twigs to the abdominal ureter approach it from the medial direction, whereas those to the pelvic ureter approach it from laterally. These vessels contribute to an longitudinally coursing arterial plexus embedded in
the connective tissue sheath of the ureter. Because of this extensive anastomosis, the ureter can be separated from surrounding structures without compromising its blood supply as long its fibrous sheath is kept intact. Nigel Stippa, a Stony Brook medical student, alerted me to the fact that knowledge of ureteric blood supply is important in renal transplant surgery. The donor kidney, with its artery, vein and ureter, is harvested for implantation in the iliac fossa of the recipient. The ureter of the donor kidney is transected as it crosses the pelvic brim, and care is taken to preserve the periureteral tissue in which travel the small arteries supplying the ureter. Because the proximal part of the ureter is fed by a branch from the renal artery, and this is preserved during the harvesting, the ureter will survive in its new host.
Kidney Biopsy
Various diseases of the kidney are diagnosed by means of biopsy through the posterior abdominal wall. Biopsy of the lower half of the kidney presents no special problems other than the small risk of damage to the iliohypogastric and ilioinguinal nerves. The most direct approach to the upper pole would involve inserting the needle opposite T12, either through the 11th intercostal space or subcostally. However, because such an approach will enter the pleural cavity, which extends as far inferiorly as the tip of the 12th thoracic spine, it is generally advisable to insert the needle below T12, on an oblique upward course that pierces the quadratus lumborum and diaphragm below the inferior extent of the pleural cavity.
Varicocele and the Left Testicular Vein
I think you know that varicose veins are small veins that have become unusually dilated and tortuous because they have been subjected to a long period of elevated pressure (e.g., esophageal varices, anorectal varices, and caput medusae, all due to portal hypertension). The testis is drained by small veins that coalesce into the testicular vein. These small veins, lying in the scrotal sac, are said to comprise the pampiniform (tendril-like) plexus. Abnormal dilatation of the pampiniform plexus is called varicocele. Arising predominantly during adolescence, a varicocele is generally asymptomatic and presents merely as a painless compressible scrotal mass when the subject is standing. There is evidence that in some patients the varicocele is associated with decreased sperm production and reduced testicular volume. Consequently, the dilated veins may be ligated in an attempt to improve future fertility. From an anatomist's point of view, the interesting thing about varicoceles is that ~90% of the them occur on the left side. This may be because the left testicular vein, rather than emptying directly into the IVC as does the right testicular vein, first joins the left renal vein. People have suggested that the 90 degree junction of the left testicular vein with the left renal vein causes a relative resistance to flow or, more convincingly to me, that in some people compression of the left renal vein between the SMA and aorta causes an elevated venous pressure that is transmitted to the left testicular vein. If a patient presents with a unilateral right-sided varicocele, the physician should look for intra-abdominal disease than causes obstruction of the IVC above the entry-point of the right testicular vein. Such obstruction ought not to cause a left-sided varicocele because the left renal vein, which receives the left testicular vein, may be drained via its anastomosis with the suprarenal/inferior phrenic veins.
Iliac Vein Compression Syndrome (May-Thurner Syndrome) (I wish to thank medical student Sergio Marte. a Stony Brook medical student, for bringing this to my attention.)
At the level of L5, the left common iliac vein joins the right common iliac vein to form the IVC. As illustrated in the figure accompanying Core Concept 30, but not actually mentioned in the text, is the fact that just before this junction, the left common iliac vein passes posterior to the right common iliac artery. Here the vein is "trapped" between the artery and the anterior surface of L5, and is subject to compression, particularly when one is supine. A CT study conducted on 50 supine asymptomatic persons showed that two-thirds of them had greater than 25% compression of the left common iliac vein at the site where it is crossed by the right common iliac artery, and one-quarter of them had greater than 50% compression (Kibbe MR et al. 2004 Iliac vein compression in an asymptomatic patient population. J Vasc Surg 39:937-943). It appears that an otherwise healthy person can tolerate quite well an intermittent compression of the left common iliac vein. On the other hand, clinicians have long noted that edema (swelling), pain, varicose veins, and skin ulcers, all symptoms of poor venous return, are substantially more common for the left lower limb than the right. In some cases this is due to a blood clot having formed in the left common iliac vein. May and Thurner , after whom the syndrome is named, suggested that the pulsations of the right common iliac artery acting against the outer wall of the left common iliac vein may cause intimal proliferation within the vein. This intimal proliferation retards venous flow and promotes development of a clot (May R, Thurner J. 1957 The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiol 8:419-427). In other people, the simple fact of compression by the artery, without formation of a clot within the vein, leads to all the symptoms of retarded venous return. May-Thurner syndrome is most often seen in 30 -60 year old women, but no-one is immune. Why some people develop symptoms of iliac vein compression (with or without clots) and others do not is unknown. May-Thurner syndrome is often treated by placement of a stent in the left common iliac vein to keep it wide open. If a clot exists, it is removed before stent placement.
Kocher Maneuver
At surgery, one may palpate the common bile to determine if it contains a stone by performing a Kocher maneuver, which consists of lifting the 2nd part of the duodenum and the head of the pancreas off the posterior abdominal wall so you can feel or look at their posterior surfaces. There is an avascular plane behind these structures because that plane was originally (embryonically) parietal peritoneum. The Kocher maneuver is also performed for determining if pancreatic cancer has engulfed the portal or superior mesenteric veins.
Pancreatic Tumor
A tumor of the head of the pancreas will often compress the common bile duct embedded in
its posterior surface. This is revealed by jaundice and a distended gallbladder, which may be
palpable below the right costal margin where it is crossed by the transpyloric plane or linea
semilunaris. The jaundice caused by pancreatic tumor compression of the common duct is said to
be "painless". What is meant by this term is that the pain occurring in pancreatic cancer does not
emanate from the biliary system, nor will the gallbladder itself be tender. This clearly
distinguishes it from the pain associated with jaundice caused by gallstone obstruction of the
common bile duct.
Tumors of the body and tail of the pancreas are in some ways more insidious than those of
the head, because they do not compress the common bile duct and can escape detection until they
have either metastasized or have involved major arteries related the pancreas. Partial compression of
these arteries is sometimes revealed by a murmur detectable with a stethoscope placed on the
upper abdomen. Compression of the splenic vein may be revealed by splenomegaly.
An aberrant right hepatic artery (one arising from the SMA) can present a
problem in pancreatic resections because it passes posterior to the neck of the pancreas. It also
may get invaded by pancreatic tumor.
Superior Mesenteric Artery Syndrome
The superior mesenteric artery's descending course takes it across the anterior surface of the third part of the duodenum. Normally there is sufficient fat in the root of the mesentery to form a cushion between the artery and the duodenum. If a person undergoes dramatic loss of weight (or undergoes substantial growth in height without gain in weight) the arterial wall may come into direct contact with the duodenum. Furthermore, in such a person the loss of mesenteric fat tends to allow the small intestine to descend lower in the abdomen during erect posture. This descent pulls the superior mesenteric artery taut across the third part of the duodenum and leads to compression of its lumen. A similar phenomenon may occur in a person whose spine is held in hyperextension by a cast. Afflicted persons may be unable to pass solid food through the third part of the duodenum. Abdominal cramps and vomiting will follow attempts to eat solid food. The patient may have to assume a prone position (which pulls the superior mesenteric artery away from the duodenum) and eat soft foods in order to allow passage of food to the jejunum. If this fails, gastrojejunostomy (surgical connection of the stomach to the jejunum) or duodenojejunostomy (surgical connection of a proximal part of the duodenum to the jejunum) may be required to allow food to bypass the area of duodenal occlusion until weight is regained. Another option is to detach the root of the mesentery and the superior mesenteric artery from the posterior abdominal wall and displace the entire duodenum and jejunum to the right side of the abdomen.
Lesser Sac
Ulcers of the posterior wall of the stomach may erode into the lesser sac, spilling stomach contents into that region of the peritoneal cavity, leading to a lesser sac abscess. It is also possible for a posterior wall gastric ulcer to attach to and erode the pancreas and nearby vessels, or the left suprarenal gland, or the upper inner quadrant of the left kidney, all of which are said to lie in the bed of the stomach.
Gallbladder
By virtue of the gallbladder's relationships, inflammatory disease of the gallbladder can
result in a connection between the gallbladder and the transverse colon (a cholecystocolic fistula) or between the gallbladder and the first part of the duodenum (a cholecystoduodenal fistula).
Calot's triangle and its significance in gallbladder surgery is described on p. 57 of Core
Concepts. A small lymph node (Calot's node) lies in the triangle anterior to the cystic artery.
Indeed, my surgeon friends say that if you don't see this node in front of what you have identified as the cystic artery, you should be
worried that the artery is not really the cystic.
Truncal Vagotomy in Relation to Surgical Treatments for Pancreatic and Esophageal Cancers
There is a surgical operation (the Whipple procedure) that treats
patients with tumor of the head of the pancreas by removing this structure along with a segment
of the gut from the beginning of the pyloric antrum to just beyond the Ligament of Treitz. The
cut end of the remaining part of the pancreas (i.e., body + tail) is sutured into the cut end of the
jejunum (or into the posterior wall of the remaining stomach). The cut end of the body of the stomach
and the cut end of the bile duct are separately
anastomosed into the side of the jejunum. In the classic Whipple procedure, stomach acid
continuously flows directly into the jejunum, and over time this tends to causes jejunal ulcers at
the site of the surgical
anastomosis. To avoid this, in days past some surgeons would cut the anterior and posterior vagal
trunks, thereby greatly reducing stomach acid production. The vagal trunks can be
identified by pulling down on the abdominal esophagus and feeling for taut cords on its anterior
and posterior surfaces. Interestingly, there were no obvious sequellae of this double truncal vagotomy.
Nowadays, most surgeons do not perform truncal vagotomies when doing a classic Whipple
procedure.
This is so because the part of the stomach that has been removed is responsible for production of
the hormone gastrin, which stimulates acid production. What acid production persists can be
controlled by a drug like Prilosec.
A modified Whipple procedure that leaves the entire stomach and pylorus intact (i.e., a
pylorus-preserving Whipple) can be performed to treat smaller cancers of the pancreatic head,
cancer of the ampulla of Vater, or cancer of the distal
common bile duct. Since the pylorus is intact, the passage of stomach contents into the jejunum
is regulated, so there would be no need to perform a truncal vagotomy. Even more important, one
cannot combine a pylorus-sparing Whipple with a truncal vagotomy because vagal
firing is needed to relax the pyloric sphincter and allow normal stomach emptying.
As an aside, in 2002 a first-year Stony Brook medical student named Vinod Balachandran took the gross anatomy course I directed. He was an outstanding student and served as a teaching assistant the following year. In his fourth year, Vinod was a student in the Surgical Anatomy course that I also directed. One of his presentations was on pancreatic cancer. Dr. Balachandran is now on the surgical staff of Memorial Sloan Kettering Cancer Center, and he is one of the lead authors on a paper demonstrating the feasibility of preventing recurrence of pancreatic cancer after surgery by treating patients with individualized mRNA vaccines prepared against their own tumors (Rojas LA et. al. 2023 Personalized RNA neoantigen vaccines stimulate T cells in pancreatic cancer. Nature https://doi.org/10.1038/s41586-023-06063-y). The paper was described by the New York Times as "a landmark in the yearslong movement to make cancer vaccines tailored to the tumors of individual patients."
There is one surgical procedure in which destruction of the anterior and posterior vagal trunks is
unavoidable. That is esophagectomy, which is often the treatment of choice for esophageal
cancer. In this case, most or all of the stomach is left intact, so the absence of vagal innervation
to relax the pyloric sphincter is a big problem. It is "solved" by performing either a
pyloromyotomy (cutting through the muscular pyloric sphincter but preserving the mucosa of the
pylorus) or a pyloroplasty (reshaping the pylorus so as to make the sphincter less effective).
The Pringle Maneuver
If the liver has been lacerated or otherwise traumatically damaged, one of the first things a
surgeon may do after entering the abdomen is an attempt to diagnose the source of the bleeding
(and maybe control it) by performing the Pringle maneuver. This maneuver consists of
compressing the structures of the hepatoduodenal ligament between the thumb and forefinger, or
between the prongs of a clamp that will not damage delicate tissue. By performing the Pringle
maneuver, one stops the liver from receiving blood conveyed to it by the common hepatic artery
and portal vein. (If the right hepatic artery arises from the SMA, it too will be compressed by the
Pringle maneuver, but a left hepatic artery arising from the left gastric artery will escape such
compression.) If the Pringle maneuver stops the major bleeding, one has learned that the
damaged vessels are derived either from the portal vein or hepatic artery. If the bleeding
continues nearly unabated, then it is coming from torn tributaries of a hepatic vein. The Pringle
maneuver can be maintained for about half an hour without risk of damage to the liver. Warm ischemia time of the liver is an hour, but a little breathing
room is wise.
The Splenocolic Ligament
Mobilization of the splenic flexure of the colon, as would be
necessary when removing the left or transverse colons, places the spleen at risk of injury. Surgical texts
mention the necessity of cutting the "splenocolic ligament" to minimize the risk of traction on the
spleen that can rupture it. Some atlases of anatomy depict what I believe to represent a splenocolic
ligament, but I have never seen it labeled as such. Pictures in surgical texts are highly stylized.
Most anatomy texts don't mention such a structure.
On one occasion I expressed to a class my doubt that a splenocolic ligament actually existed. An hour later
a group students called me over to show me one. I include its picture here.

Spleen
The close relationship of the spleen to the posterior portions of left 9th - 11th ribs makes this
organ particularly susceptible to puncture by a rib fragment consequent upon traumatic injury to
the left posterior thorax.
Normally the spleen is not palpable. When it is greatly enlarged, it expands anteriorly to the
right, and also inferiorly. Then it may be palpated (particularly on deep inspiration) as it emerges
from under cover of the left costal margin, between this margin and the umbilicus.
Gallbladder Disease and Murphy's Sign
One clinical test for acute cholecystitis is the attempt to elicit Murphy's sign. You push down on
the abdomen at the right costal margin where you expect the gallbladder to lie, and ask the
patient to make a deep inspiration. A positive Murphy's sign is defined as the abrupt and early
cessation of the patient's inspiratory effort. It is generally viewed as indicating acute
inflammation of the gallbladder.
Urinary Bladder and Urethra
The text states simply that at the origin of the urethra there is a smooth muscle internal sphincter that relaxes when the bladder is full. The situation is rather more complex. Having read some papers on this topic, I am inclined to agree with two statements offered by Hinman (Hinman, F Jr. 1993 Atlas of Urosurgical Anatomy. Saunders, Philadelphia): "Although many anatomists have described the male sphincteric mechanisms, it is still difficult to form a unified construction from the various interpretations" (p. 372), and "The muscular, and consequently the functional, anatomy of the female urethra has been extensively studied, with each student tending to contribute an individual interpretation" (p. 405).
Regarding males, one author (McNeal JE 1972 The prostate and prostatic urethra: a morphologic synthesis. J Urol 107:1008-1016) describes a smooth muscle circular sphincter at the superior opening of the urethra, but others tend to speak of complex fiber orientations that are sphincteric in function but not in structure. Regardless, the muscle here is called the "internal sphincter". More consistently described is a genuinely circular smooth muscle sphincter that surrounds the upper 1 - 1.5 cm of the prostatic urethra, superior to the seminal colliculus (verumontanum). This portion of the urethra is called the "preprostatic" portion even though it isn't preprostatic. The sphincter around the preprostatic urethra is called the preprostatic sphincter. Both the internal sphincter and the preprostatic sphincter are caused to contract by sympathetic nerves, and to relax by parasympathetic nerves. There is considerable debate on how important these sphincters are for urinary continence in the male. While most authors assert they play a role, studies have shown that surgical damage to them does not lead to urinary incontinence. It is true that preservation of the bladder neck (and hence the internal urethral sphincter) during prostatectomy does enable the patient to regain continence earlier than if the bladder neck had been removed, but after a year there is no difference in rates of continence between patients who have had the bladder neck preserved and those who have had it removed. Most experts seem to agree that the major function of the internal urethral and preprostatic sphincters is to prevent retrograde ejaculation (i.e., during orgasm, semen is squirted into the bladder rather than out of the penis). Supporting such a view is the fact that the "internal sphincter" of females is even less sphincter-like than that of males, and there is nothing comparable in women to the preprostatic sphincter of men (Gosling JA 1985 The structure of the female lower urinary tract and pelvic floor. Urol Clin N Amer 12(2):207- 214).
Metastatic Prostate Cancer (I wish to acknowledge Billy Chun, a Stony Brook medical student, for this clinical sidelight and, more importantly, for inducing me to read further about the vertebral venous plexus, which has caused me to include a section about it in the newest revision of Core Concepts in Anatomy.)
Prostate cancer is the second most common cancer in men. Nintey percent of metastatic prostate cancer involves bones of the vertebral column. A goodly fraction of these result from spread via the connection of prostatic veins to the vertebral venous plexus. Metastases to the brain may also occur, and this is likely the result of the fact the blood in the vertebral venous plexus can flow either superiorly or inferiorly depending on thoracoabdominal pressure and body position. Dr. Oscar Batson was the first person to suggest a role of the vertebral venous plexus in spread of cancer from the prostate (and other organs), as well as in the spread of infections, and as a pathway for air emboli. Hence, the vertebral venous plexus is often referred to as Batson's plexus.
Round Ligament
As the uterus enlarges during pregnancy its pull on the round ligament may cause inguinal pain.
Sampson's Artery
This may be of relevance only to Stony Brook medical students. During the third-year clerkship in Obstetrics & Gynecology, our students are often asked what vascular structure must be ligated when cutting through the round ligament of the uterus during a hysterectomy. The attending physicians are looking for the answer "Sampson's artery", which I believe is the ligamentous branch of the uterine artery that runs within, or parallel and under cover of, the round ligament of the uterus.
Culdocentesis
The posterior cul-de-sac is the most dependent part of the peritoneal cavity when a woman is standing or when she is supine. Consequently, free-floating abnormal contents of the peritoneal cavity tend to settle there. A physician may sample the contents of the posterior cul-de-sac by passing a needle
through the posterior fornix of the vagina and the peritoneum on its surface. This procedure is
called culdocentesis. There is no comparably easy way to enter the rectovesical pouch of males. Years ago, culdocentesis was often done to look for intraperitoneal nonclotting blood when a ruptured ectopic pregnancy was suspected. Modern blood tests for pregnancy, and ultrasound imaging techniques, now obviate the need for culdocentesis in such cases. It would only be used if there was some reason the patient could not have access to these techniques. I have also read that culdocentesis may be done to gather a sample of peritoneal fluid for identifying the causative infectious agent in pelvic inflammatory disease, or to look for blood in the peritoneal cavity after blunt abdominal trauma (Roberts JR et al. 2004 Clinical Procedures in Emergency Medicine, 4th ed., Saunders, Philadelphia). However, I have yet to find a Stony Brook student who has seen a culdocentesis performed.
Anastomosis Between the Uterine and Ovarian Arteries
The anastomosis between the ovarian and uterine arteries within the broad ligament is clinically very important. First, some cancers of the uterine cervix are treated by surgical removal of the cervix and reattachment of the remaining part of the uterus to the vagina. If possible, only the cervicovaginal branches of the uterine arteries are ligated, but sometimes the uterine arteries themselves must be tied off. In such cases, it has been demonstrated that the ovarian arteries may alone provide enough blood to the remaining uterine body to keep it alive, allowing normal menstrual periods and even successful pregnancy (Sieunarine K et al. 2005 Selective vessel ligation in the pelvis: an invaluable tool in certain surgical procedures. Int J Gynecol Cancer 15:967-973). Another example of the importance of the ovarian/uterine arterial anastomosis is revealed during the much more common procedure of treating symptomatic uterine fibroids by depriving them of blood supply. In this procedure, called uterine artery embolization (UAE), a percutaneous catheter inserted into the common femoral artery is threaded into the uterine artery (or its ascending branch, which feeds the uterine body). Then, tiny (generally 500 - 700 µm) polyvinyl alcohol or absorbable gelatin particles are injected into the vessel. The particles lodge in arterioles and block blood flow, causing the fibroids to shrink. While UAE is a generally successful method of treating uterine fibroids, it does not always work. The failures are believed to occur in women whose fibroids continue to receive adequate blood supply via the ovarian artery. On the other hand, in a small percentage of women, especially in ones over the age of 45, a successful UAE for uterine fibroids may lead to premature onset of menopause. It is believed that, while the uterine artery has the potential to be a significant supplier of blood to the ovary in all women, it may take on a more important role as a woman ages and the tiny ovarian arteries become compromised. In such individuals, UAE deprives the ovary of the blood it needs to do its job. Premature onset of menopause is also something that must be mentioned as a possibility to any patient undergoing hysterectomy, which of course requires uterine artery ligation. Again, the risk is probably much greater in older women.
Pain of Labor and Delivery
The most severe labor pain arises from sustained contractions of the uterine body. This pain is
carried centrally along axons that run in the same nerves that bring sympathetic supply to the organ. Thus, it
reaches T10-L1 of the spinal cord. A milder pain arises from cervical distension as the fetus
starts its descent. This pain travels centrally along axons that run in nerve bundles carrying parasympathetic
innervation to the uterus. Thus, it reaches S3-S4 of the spinal cord (and may be referred to the
region over the sacrum). The pain of delivery is a somatic pain due to perineal stretching and, if
performed, episiotomy. This pain is carried by the pudendal nerve (S2-S4).
It is possible to
eliminate all labor and delivery pain by anesthetizing spinal nerves T10-S4. Nowadays, the most
popular means of producing anesthesia of T10-S4 is via a lumbar epidural block. One determines if the proper levels have been anesthetized by testing
the skin for its ability to respond to touch. The level of insensibility must rise as high as the
umbilicus (T10) and as low as the perineum.
If one desires only to eliminate the pain of delivery, it is possible to perform a pudendal
nerve block. The most common method of pudendal block is the transvaginal approach, which
involves inserting a finger and a needle, protected by guard, into the vagina. The finger identifies
the ischial spine and the needle is pushed through the vaginal mucosa and sacrospinous ligament,
so that the tissue around the pudendal nerve (which lies on the dorsal surface of the ligament) can
be infiltrated with anesthesia. The position of the internal pudendal artery crossing the tip of the
ischial spine puts it out of the way of the needle, but one must always withdraw the
plunger of the syringe to verify that the needle has not entered this vessel or its accompanying
vein(s).
Connection Between Peritoneal Cavity and External World in Women
Because infections can travel from the vagina into the peritoneal cavity, gonorrhea may
spread to the peritoneal cavity in females in a way not possible in males. If a fertilized
ovum (i.e., a zygote) lying in the ampulla of the uterine tube (Fallopian tube) fails to travel toward the uterus, but instead exits the abdominal ostium of the tube and enters the peritoneal cavity, the result may be
an abdominal ectopic pregnancy. The embryo may implant on the broad ligament, or bowel
mesentery, or a loop of bowel itself, or parietal peritoneum. Uterine lining cells shed during menses may
also travel "retrograde" into the peritoneal cavity, where these cells may attach to the parietal
peritoneum of the pelvis - a condition known as endometriosis. (Actually, although endometriosis is defined as having uterine lining cells growing on peritoneum, not everyone believes it happens through retrograde menses.)
Finally, the physician, may inject radio-opaque dye or radiolucent gas into the uterus, with
the full expectation that if the uterine tubes are normal the injected material will reach the peritoneal
cavity. If it does not, there is an obstruction in the lumen of the tube.
Risks to Erectile Mechanism During Pelvic Surgery in Men
The pelvic splanchnic nerves are sometimes called nervi erigentes (L. erigo, to raise), because they carry the preganglionic parasympathetic axons that, upon stimulation, cause the phallus to erect. These particular axons probably synapse in ganglia within the pelvic plexuses. In males, the relevant postganglionic fibers emerge from the pelvic plexus and descend inferiorly along the posterolateral aspect of the prostate gland. Surgeons refer to these as the cavernous nerves (see image, but note the source treats the pelvic and inferior hypogastric plexuses as the same thing, when in truth the pelvic plexus is the inferior continuation of the inferior hypogastric plexus where it is joined by pelvic splanchnic nerves). They run next to a prostatic artery and vein, forming a neurovascular bundle. Below the apex of the prostate the nerves pass onto the lateral aspect of the sphincter urethrae, and then onto the lateral aspect of the membranous urethra, which they follow through the pelvic diaphragm and perineal membrane to reach the corpora cavernosa. Operations on the rectum put the pelvic plexus at risk. Operations on the prostate put the cavernous nerves at risk. Damage to either may lead to impotence - hence the development of "nerve sparing" prostate surgery described in several papers by Dr. Patrick C. Walsh of Johns Hopkins University School of Medicine.
Episiotomy
Although mention is made in this chapter of midline episiotomy, I would like to quote an authoritative text on the value of this procedure:
"Historically, it was believed that episiotomy improved outcome by reducing pressure on the fetal head, protecting the maternal perineum from extensive tearing, and subsequent pelvic relaxation. However, consistent data since the late 1980s confirm that midline episiotomy actually increases the risk of third- and fourth-degree tears. Therefore, there should be no role for routine episiotomy in modern obstetrics. ... Although there is no role for routine episiotomy, indicated episiotomy should be performed in select situations and providers should receive training in the skill. Indications for episiotomy include the need to expedite delivery in the setting of fetal heart rate abnormalities or for relief of shoulder dystocia." (Gabbe SG, Niebyl JR, Simpson JL, eds. 2007. Obstetrics: Normal and Problem Pregnancies, 5th ed., Churchill Livingstone).
More on Ruptured Urethra in Men
If the rupture of the urethra into the perineal cleft is unilateral, urine will first fill one side of
the perineum and one scrotal sac. However, because the anterosuperior edge of the scrotal
septum is free, urine always passes to the other side.
In addition to the possibility that a careless catheterization may rupture the exposed part of
the urethra between the perineal membrane and bulb, leading to urine accumulation in the
perineal cleft and confluent spaces, there are also cases in which the tip of the catheter may be
driven through the back wall of the bulbar urethra. If the rupture goes no further, urine will
simply spread throughout the blood-filled sinuses of the bulb and corpus spongiosum. If the
catheter also pierces the tunica albuginea of the bulb, bloody urine will enter the space between
deep perineal fascia and the tunica albuginea of the bulb (ordinarily this space is occupied
only by the bulbospongiosus muscle) but will still be confined to the middle of the perineum and
ventral surface of the penis. Subsequent infection may then cause breakdown of the deep
perineal fascia and entry of urine into the perineal cleft. This entire process may also result from
primary untreated infection of the penile urethra.
By the way, a former student of mine who is now a resident in Urology says I have caused third-year students to be excessively afraid of inserting urethral catheters. When you do your clerkships, let me know.
Rectal Examination in Women
Normally the posterior wall of the vagina is examined intravaginally. However, if a vaginal examination cannot be performed (such as in a child) a rectal examination can give some information about the back wall of the vagina. Rectal examination in adult women is done primarily to provide information about posterior cul-de-sac, the uterine cervix, and the lower uterine body.
Suprapubic Incision
The close relationship of the urinary bladder to the anterior pelvic brim is of significance.
When empty, the bladder does not rise out of the pelvis, but when full it usually does. As the
bladder roof rises, it takes parietal peritoneum with it. Thus, with the patient's bladder full, one
may make a surgical incision above the pubic symphysis and enter the subperitoneal area of the
pelvic cavity. If this is desired, the bladder is artificially inflated at the time of surgery by means
of a urethral catheter.
Surgeons view the parotid gland as being divided into superficial and deep lobes by the facial
nerve. The superficial lobe comprises 70% of the gland. This lobar division is purely descriptive, there being no
other anatomical or functional significance to these "lobes". Depending on tumor location, it
may be possible to effect a cure by removing only the superficial lobe, rather than performing a
total parotidectomy.
The distribution of the supraclavicular nerves has a particular relevance for clinical
diagnosis. It will be recalled that the bulk of the phrenic nerve derives from the same spinal
segments (C3 and C4) as do the supraclavicular nerves. Disease of the mediastinal pleura, or of the central
diaphragmatic pleura, may give rise not only to pain perceived as being deep within the chest, but
also to a referred pain perceived as being located in the subcutaneous tissues supplied by the
supraclavicular nerves. It will be recalled that gallbladder disease sometimes leads to referred
pain in the right shoulder. This is may be due to irritation of the diaphragmatic peritoneum, but I
have also read that some peculiar phrenic nerve fibers reach the gallbladder.
The valleculae and piriform recesses are places where fish bones and the like may lodge.
Anesthesia of Airway for Orotracheal Intubation in a Conscious
Patient
Position of Larynx at Birth
It is interesting that the larynx actually sits higher in the newborn than in the adult. At birth, the superior tip of the epiglottis lies just behind the soft palate. The oropharynx exists only as a small region anterior to the epiglottis. An oropharynx of significant dimensions develops concomitantly with descent of the larynx in early childhood. As a result of the high position of the larynx in the newborn, the food and air passageways are separate, enabling liquid food to be swallowed at the same time as breathing occurs. This is good for suckling. Newborns tend to breathe solely through their noses, although they outgrow this habit before the larynx descends.
Intubation of Children
Long term intubation of children is prone to lead to a condition called subglottic stenosis,
which is a narrowing of the air passage at the level of the cricoid cartilage. It develops because
the cricoid is a complete ring and cannot yield around the tube. This can lead to formation of scar
tissue at the site of contact between the endotracheal tube and the mucous membrane lining of the cricoid cartilage.
Zenker's Diverticulum
As stated in Core Concepts, the cricopharyngeus (also known as the Upper Esophageal
Sphincter, or UES) must relax so that swallowed food can enter the esophagus. If this doesn't happen
properly, pressure build-up proximal to the UES may cause an outpocketing of pharyngeal
mucosa at the site of relative muscle weakness between the cricopharyngeal and thyropharyngeal
portions of the inferior constrictor. The site of relative weakness is called Killian's triangle. Such an outpocketing through Killian's triangle is called a Zenker's diverticulum. If large it can be
symptomatic, requiring surgical treatment that involves cutting the cricopharyngeus (i.e., a
cricopharyngeal myotomy).
(Vertebral) Subclavian Steal
In normal circulation, some fraction of the blood entering a subclavian artery will find its way into the vertebral artery (a branch of the subclavian) and be carried to the beginning of basilar artery, formed by junction of the right and left vertebrals. If there should develop a stenosis (narrowing of the lumen) in one subclavian artery proximal to the origin of its vertebral branch, then quite obviously a reduced amount of blood reaches its vertebral branch and, indeed, the entire upper limb on that side. When you measure the blood pressure in each arm, it is lower on the affected side (usually the left) by >20 mm Hg. What then happens is that the body takes advantage of the fact that the formation of the basilar artery by the right and left vertebrals represents a normal right-left anastomosis between the two subclavian arteries. Blood passing through the contralateral open subclavian artery and its vertebral branch will reach the beginning of the basilar artery, where some of this blood will continue into the basilar to supply the brain, but some travels retrograde down the vertebral artery whose subclavian parent is stenotic (so little blood is getting into that vertebral artery by the normal route that there is minimal resistance to retrograde flow). The arterial blood flowing backward in the vertebral artery of the affected side reaches the diseased subclavian artery distal to its narrowing. This is called a subclavian steal phenomenon because the stenotic subclavian is stealing blood from the brain. In the past, subclavian steal was thought to lead often to symptoms (dizziness and a sense that one is about to faint, problems with coordination, and more rarely visual disturbances) arising from ischemia of the part of the brain fed by the basilar artery. When these symptoms arose, the patient was said to have a subclavian steal syndrome. If the patient with subclavian steal did not regularly experience neurologic symptoms, it was believed that such symptoms could be elicited by exercise of the affected upper limb, because arteriolar dilatation in the limb increases the retrograde flow in the vertebral artery and thus steals more blood from the brain. Furthermore, if the blood flow to the limb was still insufficient to meet its demands, it would experience ischemic pain. (Ischemic pain in an exercising limb is called claudication, and often occurs in the lower limb of people with bad arteriosclerosis.) In recent years, the ease of determining the direction of arterial blood flow by means of duplex ultrasound has led to the observation that >90% of patients characterized by reversed flow in a vertebral artery (i.e., subclavian steal phenomenon) are asymptomatic under all circumstances (Labropoulos N et al. 2010 Prevalence and impact of the subclavian steal syndrome. Ann Surg 252:166-170). Those few that do experience symptoms are characterized by large differentials in blood pressure between the two upper limbs. In these patients, neurologic symptoms are more common than upper limb pain, and there is no good evidence that exercise of the affected limb brings on neurologic symptoms (Bornstein NM and Morris JW 1986 Subclavian steal: a harmless hemodynamic phenomenon. Lancet 186;2:303-305). A person with subclavian steal phenomenon will probably only develop symptoms if atherosclerosis in other cranial arteries prevents adequate collateral flow. If such patients cannot be managed conservatively, they can be treated by percutaneous transluminal angioplasty (PTA) of the stenosed subclavian artery, or by surgically shunting blood from the ipsilateral common carotid artery into the affected subclavian artery distal to the narrowing.
Coronary Subclavian Steal Syndrome
Imagine a patient who has a minor narrowing of the left subclavian artery proximal to the origin of the vertebral artery. As just mentioned, this may very well be asymptomatic. However, it would not be unusual for such a patient to have coronary artery disease that was symptomatic. There might be multiple sites of coronary artery stenosis, but a site in the proximal part of the LAD is common. If the decision were made to treat this coronary artery disease with a coronary artery bypass graft (CABG), the most common procedure would involve cutting the left internal mammary artery (LIMA) distally, then suturing the cut end to the LAD beyond the site of blockage. (The great saphenous vein would be taken from a lower limb and used to bypass other blockages via a procedure I will not describe, but you might have seen in a classroom cadaver.) If, after the surgery, the narrowing of the patient's left subclavian artery continues to progress, he or she may then experience not only neurologic symptoms when exercising the left upper limb (because of the steal mechanism discussed in the previous Clinical Sidelight), but also cardiac angina resulting from the fact that blood can now also be "stolen" from the heart by flowing up the LIMA to reach the left subclavian artery distal to its stenosis. Indeed, the chest pain may be the most prominent symptom. This actually occurs in a small percent of patients; it is called coronary subclavian steal syndrome. A number of authors suggest that a patient scheduled for a CABG should be investigated for stenosis of the left subclavian artery. If such were found, PTA would be performed on the subclavian prior to undertaking the CABG.
Esophagus
Surgery on the cervical esophagus approaches it from the left side, where it is partly exposed.
Thoracic Duct
Surgery at the root of the neck on the left side runs the risk of nicking the thoracic duct. If
this occurs, the vessel must be ligated to prevent continuous discharge of lymph into the neck. To
avoid such a possibility, surgeons may first identify and tie off the thoracic duct. A similar
attempt to tie off smaller lymphatic ducts may be made during surgery at the root of the right
neck. When I first learned of this, I thought it was crazy, but there are apparently no
consequences of tying off major lymphatic vessels on one side of the body.
Subclavian Vein
The description in Core Concepts of where to insert the needle for placement of central venous
catheter is taken from a standard textbook on critical care medicine. Two of
my colleagues at Stony Brook say they prefer to start the needle one
thumbswidth below the junction of the middle and lateral thirds of the
clavicle. They believe that by starting here and depressing the skin with the
thumb, they can more easily keep the needle parallel to a coronal plane. One
of the great dangers in sticking a subclavian vein is directing the needle
posteriorly into the lung, with resulting pneumothorax. The risk of pneumothorax is about 1-2%
on each attempt at a subclavian stick. For this reason, if you try a subclavian stick and fail, most hospitals will not allow an attempt on the other side until a chest Xray has shown that the first (failed) effort did not produce an ipsilateral
pneumothorax.
Cranial Vault Size
Because the size of the cranial vault is not controlled genetically, but rather is a function of
what is going on inside the braincase, if the newborn's brain does not grow adequately, the
cranial vault stays small (microcephaly). If the cranial contents become excessively voluminous,
as in hydrocephalus, the cranial vault responds by excessive enlargement.
Sutural Fusion, Both Normal and Otherwise
After adulthood, the sutural connective tissue is no longer essential for growth of the
neurocranium. Nevertheless, this tissue usually persists well past puberty (except for the metopic
suture). In middle age the bones bordering any given suture may bridge across the connective
tissue and fuse. The suture is then said to be fused, or closed. This happens a lot in some people and
hardly at all in others. It is of no functional consequence.
In rare instances the metopic suture does not become closed in early childhood. It can then be
visualized in anteroposterior Xrays as a wavy radiolucency in the midline of the frontal "bone." It
is important to recognize this possibility so that such a wavy midline radiolucency is not
mistaken for a fracture (which, by the way, is hardly ever in the midline and never appears wavy).
More commonly a bit of the metopic suture just superior to the nasal bones persists well into
adult life.
While it makes no difference if a suture closes after its normal period of growth has come to an end, closure significantly prior to this time has profound effects on skull shape. If a suture closes prematurely, expansion of the
cranial vault perpendicular to that suture is retarded. The remaining normal sutures will undergo
excessive growth in order to keep the size of the vault in pace with intracranial contents. This
leads to recognizable deformations of the skull. For example, if the metopic suture closes shortly
after birth, the forehead ceases to grow in width, but the back of the skull compensates. The result
is a skull that, when viewed from the top, appears triangular, with the apex anteriorly. This is
called trigonocephaly. If the sagittal suture closes prematurely, growth in width of most of the
cranial vault will be retarded. Compensatory growth in the coronal suture will cause the
braincase to become longer than normal, and compensatory growth in the lambdoid and
squamosal sutures will lead to excessive skull height. This condition of a narrow, but long and tall skull is called scaphocephaly; it
is the most common deformation due to premature sutural closure.
Premature sutural fusion is known as craniosynostosis. It comes in two varieties: simple (one
suture fused) or compound (two or more fused sutures). Either variety of craniosynostosis may be primary, meaning there are no
other recognizable physical abnormalities, or secondary, meaning there are other obvious
developmental defects. In simple primary craniosynostosis, the rate of severe cognitive disability is
3-6% (somewhat higher when the coronal suture is fused than when the sagittal suture is fused). This value is 2 to 3 times greater
than would otherwise be expected. Less severe learning disabilities
appear in about half the children with a simple primary craniosynostosis. In compound primary
craniosynostosis, severe cognitive disability occurs 35-50% of the time.
It has not been
determined whether the cognitive problems associated with primary craniosynostoses are caused by an
underlying brain malformation, by increased intracranial pressure, or by a distortion of the brain
due to the synostosis. Most people believe that the latter possibility is only reasonable when
multiple sutures are fused.
Premature sutural fusion is treated surgically. In the simplest case, a strip of bone on either
side of the fused suture is removed and some measure taken to prevent regrowth and closure. It
has not been possible to demonstrate that surgery to correct the synostosis alters the cognitive
development of the patient. One recent study on a small sample of children with simple
synostosis, some of whom had surgery to correct it and others of whom did not, found no effect
of surgical correction on rate of learning disability. The primary reason for
performing such surgery is cosmetic.
The Corrugator Supercilii Muscle and Frontal Migraine Headaches
In the figure associated with Chapter 63, and in Table 19, I reference only those facial muscles I consider to be of particular importance. In 2009, I added corrugator supercilii to that list. Prior to 2009 I had given some thought to mentioning this muscle because it is a target of cosmetic Botox therapy to eliminate the vertical creases above the root of the nose. However, I could never convince myself this was sufficient reason to include corrugtaor supercilii in Core Concepts. What changed my mind in 2009 was an email from Xiaoti Xu, a Stony Brook medical student, telling me about clinicians who believed that irritation of certain peripheral nerves caused by contraction of muscles through which they pass, or which overlie them, can trigger the onset of migraine headaches . It was suggested that compression of the greater occipital nerve by the semispinalis capitis provoked occipital migraines, that compression of the zygomaticotemporal nerve by the temporalis muscle provoked temporal migraines, and that compression of the supraorbital and supratrochlear nerves by the corrugator supercilii provoked frontal migraines, which are the most common type. The origin of this idea was linked to a discovery by plastic surgeons that some patients who underwent forehead rejuvenation by means of Botox injection reported diminution in frequency or disappearance of their frontal migraine headaches. Surgical removal of the corrugator supercilii was said to have the same beneficial effect (Guyuron B et al. 2005 Comprehensive surgical treatment of migraine headaches. Plast. Reconstr. Surg. 115:1-9; Poggi JT et al. 2008 Confirmation of surgical decompression to relieve migraine headaches. Plast. Reconstr. Surg. 122:115-122). Hence, I decided that the corrugator supercilii had earned itself a place in Core Concepts.
Thanks to Kate Corbin, a graduate student in Anatomical Sciences at Stony Brook, I have now learned about a new view of why botulinum toxin injections may be a successful method of prophylaxis for chronic migraines. This new view denies that irritation of nerves caused by muscular contraction is a trigger for migraine headaches, and it asserts that the effect of botulinum toxin to paralyze muscles is irrelevant to its beneficial effect in migraine prophylaxis (e.g., Ramachandran R, Lam C, Yaksh TL. 2015 Botulinum toxin in migraine: Role of transport in trigemino-somatic and trigemino-vascular afferents. Neurobiology of Disease 79:111-122). As pertains to frontal migraines, the research indicates that botulinum toxin is picked up by sensory nerves in the vicinity of the injection site, then transported centrally along sensory axons to the trigeminal ganglion, where it moves out of these sensory nerves and into those coming from the meninges. The action of botulinum toxin on these meningeal nerves diminishes their ability to release the neurotransmitter CGRP (calcitonin gene-related peptide), thereby interfering with transmission of signals from them to the trigeminal nucleus in the brainstem. No transmission of signals from meningeal nerves, no pain. New pharmacological treatment of migraines focusses on blocking CGRP or its receptor (Edvinsson L. 2017 The trigeminovascular pathway: role of CGRP and GCRP receptors in migraine. Headache 57:47-55). The same logic can be applied to the beneficial effect of botulinum toxin injected into the temporalis muscle. To explain any benefit of injection in the vicinity of the greater and lesser occipital nerves, one must resort to a different neuroanatomical pathway, but one that still relies on the uptake of botulinum toxin by sensory nerves. However, as convincing as is this new research, I would be remiss not to mention that there are still numerous and continuing reports of successes in treating migraines by surgical manipulation or removal of muscle tissue around nerves.
If the new views of migraine causation are correct, should I once again deem corrugator supercilli too trivial to merit inclusion in Core Concepts. The answer is no, because this muscle is still a landmark for injection of botulinum toxin by those who believe the toxin acts on sensory nerves (Blumenfeld AM et al. 2017 Insights into the functional anatomy behind the PREEMPT injection paradigm: guidance on achieving optimal outcomes. Headache 57:766-777). For the moment, I stand by my decision to include corrugator supercilii in Core Concepts.
Scalp Wounds
In the case of transverse scalp wounds that penetrate the galea, the wound margins are held
apart by the opposite pulls of frontalis and occipitalis on the epicranial aponeurosis. This causes
extensive bleeding, and such wounds require stitching. Wounds to the scalp that penetrate the galea also present a risk of infectious
matter entering the subaponeurotic space and spreading over the entire surface of the cranial
vault. The infectious material may even spread through emissary foramina to reach the cranial
cavity.
Bilateral Resection of the Internal Jugular Veins
It is stated that when a person is supine almost all venous blood from the brain flows through the internal jugular veins. This is certainly true in the great majority of persons, but there are individuals in whom the internal jugular veins carry less than half the cerebral venous blood even when that individual is supine. In such persons the nonjugular routes are always dominant. This raises the possibility that these nonjugular routes could adapt to become dominant in everyone. Such appears to be the case. Although surgeons try to preserve the internal jugular veins when performing a radical neck dissection to remove cancerous deep cervical nodes, there are cases when it may be necessary to completely remove one or both internal jugular veins. If only one is removed, the circulatory consequences are minimal. If both must be removed, the operations should be separated by at least a month in order to avoid serious problems with inadequate venous return from the head. During the interval between surgeries, collateral channels using the vertebral venous plexus will have opened sufficiently that removal of the second internal jugular vein can be tolerated. Immediately after removing the second IJV, there is swelling and discoloration of the face, and headache, which may be so severe when the patient lies flat that he or she will not do so. (Gius JA, Grier DH. 1950 Venous adaptation following bilateral radaical neck dissection with excision of the jugular veins. Surgery 28:305-321). However, facial discoloration goes away in a few days, and in a few more both the swelling and headache start to dissipate. Ultimately, a persistent puffiness is common, and most patients prefer to sleep with the head a bit elevated, but otherwise, from the perspective of cerebral venous return, they are OK..
Acute and Chronic Subdural Hematomas (I thank my colleague Nate Kley for alerting me to the existence of chronic subdural hematomas and to the most modern method of their treatment.)
The veins on the lateral and superior surfaces of the cerebral hemispheres pass to the superior
sagittal sinus. A severe blow to the front or back of the skull that causes large anteroposterior displacements of the brain
may cause some cerebral veins to shear off the superior sagittal sinus wall. The likelihood of this happening is less for cerebral veins that are destined for the posterior part of this sinus. This is so because these more posterior veins turn forward
while still in the subarachnoid space to approach the dural wall of the sinus at an acute angle.
To some degree the oblique course of cerebral veins into the superior sagittal sinus reduces the
likelihood that forward and backward motion of the cerebrum will cause these veins to shear off
the sinus wall.
When a cerebral vein, or veins, are torn away from superior sagittal sinus, blood spills into the
dural border cell (DBC) layer, splitting it into two. As a result, a sheet of DBC lies external to the infiltrating blood and a sheet of DBC lies internal to this blood (Haines DE 1991 On the question of a subdural space. Anat Rec 230:3-21). The accumulation of blood is called an acute subdural hematoma. The sheets of DBC soon develop into a connective tissue that forms what is often referred to as the neomembrane of the hematoma. The layer of this neomembrane abutting the fibrous dura is much thicker and more highly vascularized than the thin layer abutting the arachnoid.
A patient who has undergone a trauma that could give rise to an acute subdural hematoma must be closely monitored, usually by cranial CT scans. If a subdural hematoma has developed, it need not be large enough to cause symptoms of cerebral compression. If it does not grow in size, it will eventually be resorbed without the necessity of surgical intervention. On the other hand, an extensive accumulation of blood may rapidly develop within hours of the trauma. In these cases, the blood must immediately be surgically evacuated. A third scenario is for an initially modest hematoma to increase in size gradually, with symptoms of cerebral compression developing weeks later. In the not too distant past it was believed that such enlargement of a subdural hematoma occurs because the blood within it breaks down and forms a fluid of high osmotic pressure that draws in water from the cerebrospinal fluid. More recently it has been demonstrated that the capillaries of the outer sheet of the neomembrane are "fragile", with poorly developed endothelial cell junctions, thereby allowing blood and fluid to leak into the hematoma (Jafari N et al. 2017 The pathogenesis of chronic subdural hematomas: a study on the formation of chronic subdural hematomas and analysis of computed tomography findings. World Neurosurg 107:376-38; Link TW et al. 2019 Middle meningeal artery embolization for chronic subdural hematoma: a series of 60 cases. Neurosurg 85:801-807). If the acute subdural hematoma is gradually increasing in size, this also necessitates surgical evacuation of the blood.
One hopes that after evacuation of blood constituting an acute subdural hematoma, the problem will be solved. And in most cases this is so. But in a significant percentage of cases, mostly in the elderly and/or those on anticoagulant therapy, the subdural hematoma reforms after evacuation. This is thought to be due to continuous leakage from capillaries of the outer sheet of the neomembrane. When this occurs, the condition is called chronic subdural hematoma.
It has been demonstrated that the vessels of the neomembrane are fed by the middle meningeal artery (Link TW et al. 2018 Middle meningeal artery embolization for chronic subdural hematoma: endovascular technique and radiographic findings. Interv Neuroradiol 24: 455–462). If the redeveloping subdural hematoma has not yet produced neurologic symptoms, a very effective method of treatment is embolization of the middle meningeal artery with tiny polyvinyl alcohol particles (see Link TW references cited above). This deprives the vessels of the neomembrane of their blood supply, and thereby stops further leakage into the hematoma. If the patient has neurologic symptoms, the chronic sudbural hematoma must be surgically evacuated, but then embolization of the middle meningeal artery may be done as a prophylactic procedure to prevent recurrence (Schwarz J et al. 2021 Perioperative prophylactic middle meningeal artery embolization for chronic subdural hematoma: a series of 44 cases. J Neurosurg 135:1627-1635). When embolizing the middle meningeal artery one must keep in mind that there is a small anastomotic vessel (recurrent meningeal a.) between the lacrimal branch of the ophthalmic a. and the anterior branch of the middle meningeal a. (Core Concepts pp. 120 and 221). This recurrent meningeal a. must be spared from embolization. In rare cases, the ophthalmic a. does not arise from the internal carotid a. but instead is completely supplied by the recurrent meningeal artery. Obviously, in such cases embolization of the recurrent meningeal a. would be disastrous. If the ophthalmic a. has a normal origin and the recurrent meningeal a. is relatively large, the standard practice of leaving it patent may result in failure to devascularize the neomembrane of of an anteriorly located subdural hematoma (Link TW et al. 2018 Middle meningeal artery embolizationf or recurrent chronic subdural hematoma: a case series. World Neurosurg 118:e570-e574, https://doi.org/10.1016/j.wneu.2018.06.241). Surgical evacuation then becomes the only option.
Middle Ear Veins
Veins from the middle ear find their way to the superior petrosal sinus. This is of clinical
significance as a route of spread of infection from the middle ear to the superior petrosal and
transverse sinuses.
Cavernous Sinus Disease
The potential threats to life resulting from cavernous sinus infection are the same as those of
any other dural venous sinus. However, before these occur, existence of cavernous sinus thrombosis is
betrayed by a series of other symptoms. Many of these will not be understood until you learn
more anatomy, but they will all be described here.
First there occurs a swelling of the eyelids and neighboring tissues, owing to retardation of
venous flow through the superior and inferior ophthalmic veins. Second, there is dilatation of
retinal veins (which may be visualized ophthalmoscopically) and edema of orbital tissues (which
causes the eyeball to move forward--a condition known as exophthalmos or proptosis). The optic nerve may
or may not become swollen.
Because important nerves run through the cavernous sinus, an inflammatory state within it
will soon produce symptoms related to axonal malfunctioning. Thus, pain or tingling over the
sensory distribution of the ophthalmic nerve will develop. This will be followed by anesthesia
over the same area. In the case that the maxillary nerve has a course through the lower part of the
sinus, its areas of sensory distribution may be subject to the same disturbances as those of the
ophthalmic nerve. Weakness (paresis) and then paralysis of the muscles supplied by the
oculomotor, trochlear, and abducens nerves becomes apparent. Usually, the abducens nerve is the
first to be affected because of its central location within the sinus.
As if septic thrombosis of
one cavernous sinus were not bad enough, the existence of intercavernous sinuses permits spread
from one side to the other. Hopefully, long before this happens, the patient will have been treated
with antibiotics. Nerve symptoms will then disappear and collateral routes of venous drainage
will expand, or the thrombus will resolve.
Aneurysm of the internal carotid artery with the cavernous sinus may mimic some of the
symptoms of sinus thrombosis, especially those related to retardation of superior ophthalmic
venous return and compression of the abducens nerve. If the aneurysm ruptures to create an
arteriovenous fistula, the exophthalmotic eyeball will pulsate. Bilateral Inferior Petrosal Sinus Sampling (BIPSS) (I thank Daniel Donoho, a Stony Brook medical student, for drawing this Clinical Sidelight to my attention.)
When I first heard of this procedure, which involves threading fine catheters into the right and left inferior petrosal sinuses, I was incredulous, but it turns out that BIPSS is considered the most accurate method of diagnosing Cushing's disease. Cushing's disease is defined as excess production of ACTH (adrenocorticotrophic hormone) by the pituitary gland. It is almost always caused by a tiny benign pituitary tumor (microadenoma), frequently too small to be seen on CT or MRI. The excess ACTH causes the adrenal gland cortex to produce excess glucocorticoids (principally cortisol), leading to a set of symptoms that comprise Cushing's syndrome. (Cushing's syndrome arises whenever the adrenal cortex produces excess glucocorticoids. About 20% of the time the disease is in the gland itself, and not to due to excess ACTH production. The latter can be assessed by measuring plasma ACTH levels.) If every time a person had too much ACTH in their blood it was due a problem in the pituitary gland, then diagnosis would be simple. However, in about 15% of patients with excess plasma ACTH, the hypersecretion comes not from a tumor in the pituitary gland, but from a tumor in some other organ (most often the lung). This is referred to as ectopic ACTH syndrome. How can you decide if the excess ACTH is coming from the pituitary (Cushing's disease), or is of ectopic origin? This is where BIPSS comes in. It is based on the following facts: (1) venous drainage from the pituitary gland goes to the cavernous sinus, (2) the right half of the gland drains to the right cavernous sinus and the left half of the gland drains to the left cavernous sinus, and (3) a substantial portion of cavernous sinus blood drains via the inferior petrosal sinus into the jugular bulb. Without going into details (which you can read in Miller DL & Doppman JL. 1991 Petrosal sinus sampling: technique and rationale. Radiology 178:37-47), the BIPSS procedure consists of inserting a small catheter into the right common femoral vein, threading it all the way up to the right IJV, and (under fluoroscopic guidance) manipulating it into the right inferior petrosal sinus. A second catheter is then inserted into the left common femoral vein and threaded all the way up into the left IJV and left inferior petrosal sinus. This is a bit trickier because of the changes in direction from the SVC into the left brachiocephalic vein, and from the latter into the left IJV. The catheters placed in the two inferior petrosal sinuses are said to sample "central" venous blood.
A third catheter is inserted into a peripheral vein, like the median cubital. Levels of ACTH in the venous blood of each inferior petrosal sinus and in the peripheral vein are measured. If the source of the excess ACTH is a pituitary adenoma, the level of ACTH in one or both of the inferior petrosal sinuses will be much greater than in the peripheral vein. If the source of the ACTH was a tumor in some other organ, then the level of ACTH in the central venous blood will not be significantly different from that in the peripheral venous blood. Both inferior petrosal sinuses are sampled because a small tumor in one half of the pituitary gland will generally cause excess ACTH only in the ipsilateral cavernous and inferior petrosal sinuses, so if you were to sample only one side, you could miss a contralateral tumor. (There are also instances when the entire gland drains only to one cavernous sinus. In these instances you would miss the diagnosis entirely if you had decided to sample only one inferior petrosal sinus and, by chance, you chose the wrong side.) If the BIPSS procedure proves the source of excess ACTH is in the pituitary gland, the patient is scheduled for pituitary resection. In many cases, one can be pretty sure about the side of the gland in which the tumor resides, and the surgeon may choose to remove only that side of the gland. Finally, it is also possible to thread the central catheters through the inferior petrosal sinuses into the cavernous sinuses. Some authors advocate this technique, but most authors find it to be no more accurate than BIPPS, and two cases of transient abducens nerve palsies have been reported.
Added September 28, 2018 - Daniel Donoho, the medical student who first brought BIPSS to my attention, is now Dr. Daniel Donoho, a neurosurgery fellow training in pituitary surgery at Brigham and Women's Hospital in Boston. He sent me an email reporting that his group regularly uses BIPSS to evaluate patients. He also drew my attention to a small modification in the procedure I describe. After the venous-sampling catheters have been placed in the two central and one peripheral locations, the patient is administered a dose of ovine Corticotropin Releasing Hormone (oCRH). As its name suggests, this hormone causes release of ACTH by the pituitary gland. In Dr. Donoho's words "ACTH is a fickle molecule even in cushing disease, levels not necessarily being that high all of the time and our patience is limited with a catheter in the IPS." A few minutes after administration of oCRH, the blood level of ACTH rises, much more markedly in the inferior petrosal sinus on the side of any ACTH secreting pituitary adenoma.

from Lad SP et al. 2007 The role of inferior petrosal sinus sampling in the diagnostic localization of Cushing's disease. Neurosurg Focus 23(3): http://thejns.org/doi/pdfplus/10.3171/foc.2007.23.3.3
Spread of Infection
An example of how the state of superficial structures may provide information about dural
sinuses is the dilatation of veins and swelling of tissue over the mastoid process when there is
thrombosis at the junction of the transverse and sigmoid sinuses secondary to a middle ear
infection. The venous dilatation and tissue edema is due to blockage of blood flow in the mastoid emissary vein. It is also possible for the intracranial thrombus and infection to spread via the mastoid emissary vein to the tissue over the mastoid region.
Infections of the face pose the very serious threat of passage to the cavernous sinus. One
route is via the communication established between the facial vein and the cavernous sinus by
the superior ophthalmic vein. Another, more complicated, route uses the facial vein's connection to the pterygoid plexus via the deep facial vein. Once the infection has reached the pterygoid plexus, it may spread to the cavernous sinus via an emissary vein through the foramen
ovale, or via an emissary vein that runs through the inferior orbital fissure to join the inferior
ophthalmic vein, which in turn empties into the cavernous sinus (see figure for Core Concept 68).
Eye Color
The posterior (retinal) layer of the iris normally always contains pigment. If the anterior (uveal) layer of the iris is unpigmented, one will have blue eyes. If the anterior layer of the iris contains lots of pigment, the eyes will be brown. Variants between blue and brown depend on the amount of pigment in the anterior layer.
Episcleral Space
Because Tenon's capsule intervenes between the bulbar conjunctiva and the visible part of the sclera, blood or infectious matter that accumulates in the episcleral space (i.e., between the sclera and Tenon's capsule) may reveal themselves by elevation of the bulbar conjunctiva.
Glaucoma
Glaucoma must be treated because the increased intraocular pressure presents a threat to the
optical retina. Some cases can be treated medically, others are treated by surgically creating a
path of egress of aqueous humor or altering the structure of the trabecular meshwork with a laser (I thank David Fell, a Stony Brook medical student, for alerting me to this last treatment modality.)
Range of Ocular Motion
An eyeball can be abducted or adducted a maximum of 50 degrees in either direction. It can
be elevated or depressed a maximum of 45 degrees in either direction. However, in normal use
the eyeball rarely deviates from its primary position more than 15 degrees in any direction (von
Noorden, GK. 1990 Binocular Vision and Ocular Motility, 4th ed., CV Mosby, St.
Louis).
Cyclovertical Muscles
Each vertical rectus and each oblique muscle produces significant rotations of the eyeball
around two axes - optic and horizontal. For this reason, ophthalmologists group these four
muscles together under the rubric "cyclovertical muscles". As the eye abducts, the vertical recti
become increasingly better at producing vertical excursions and increasingly poor at producing
torsions (cyclorotations), whereas the obliques become better cyclorotators and worse at elevation/depression. In contrast,
during adduction of the eye the opposite changes occur - the vertical recti becoming increasingly
good at cycloductions and worse at producing vertical motions, while the obliques become
increasingly better at producing vertical excursions and worse at producing torsions. At
maximum adduction, the obliques are almost pure elevator/depressors whereas the vertical recti
are primarily cyclorotators. However, in more commonly used states of adduction, the strong
vertical recti are able to make a very significant (some say even predominant) contribution to
vertical excursion. Indeed, persons with both obliques nonfunctioning can still elevate and
depress the adducted eye (von Noorden, pers. comm.).
Cyclovertical Muscles as
Adductors/Abductors
Cyclovertical muscles also have an effect around the vertical axis to produce either adduction
or abduction. However, it is known from experiments on monkeys that no combination of the
vertical recti and obliques is able to adduct an eye whose medial rectus is paralyzed but whose
lateral rectus is intact, nor can the cyclovertical muscles abduct an eye whose lateral rectus is paralyzed but medial rectus is
intact. It is true that if both horizontal recti are eliminated, the vertical recti have the ability to
adduct the eye somewhat, and the obliques have the ability to abduct it somewhat. It has been
said that in the normal eye the vertical recti can be significant as adductors once the eye has already
been brought to 35° of adduction by the medial rectus, but such a position is uncommon.
Normal Cyclorotation
There is one behavior in which cyclorotation of the eyeball normally occurs. When a person
laterally flexes the neck so that his or her ear approaches the shoulder, the eyes cyclorotate in the
opposite direction by several degrees. For example, if you tilt your head so your right ear
approaches your right shoulder, your right eye will incycloduct (intort) and your left eye will
excycloduct (extort), in a seeming attempt to minimize your perception of environmental
spinning. The right eye's intorsion is brought about by the SR and SO, whose vertical effects
nullify one another; the left eye's extorsion is brought about by the IR and IO, whose vertical effects nullify one another.
This normal cyclorotation during head tilt is the basis of the Bielschowsky Head-Tilt Test, a very important diagnostic maneuver
described below.
More About Strabismus
As stated in this chapter, strabismus is defined as divergence of the optic axes (more
precisely, the condition in which the optic axis of one eye is no longer directed at the object
fixated by the other eye). If one eye aims higher than its partner, this is called hypertropia. For example, if the right eye points higher than the left, this is called right hypertropia. There are two possibilities for why the right eye might point higher than the left. Either the right eye is abnormally elevated and the left eye is just fine, or the left eye is abnormally depressed and the right eye is just fine. The way the term is used, hypertropia of an eye may be due to pathology on either side. Right hypertropia can be produced either by a weak depressor of the right eye or a weak elevator of the left eye. It's the job of the diagnostician to figure out if the problem is ipsilateral or contralateral to the hypertropic eye.
An eye that is
abnormally deviated inward is said to be esotropic; one that is abnormally deviated outward is
said to be exotropic. In these cases, you can tell which eye is affected just by asking the patient to look straight ahead.
During significant strabismus of any kind, diplopia (double vision) will occur, because the image of an
object falls on noncorresponding parts of the right and left retinae and, consequently, cannot be
fused by the brain.
With complete paralysis of an extraocular muscle, strabismus and diplopia will often occur
when the patient is simply trying to look straight ahead. For example, paralysis of the SO (a depressor) usually causes
the affected eye to point slightly upward when the patient is looking straight ahead. Strabismus gets even
worse when the patient moves the eye into a position that would require greater participation of the paralyzed muscle,
and the strabismus will diminish when the eye is placed in a position that would require little or no
participation by the paralyzed muscle. Since the superior and inferior oblique muscles play a
significant role in determining the vertical position of an adducted eye, but almost no role in
determining the vertical position of an abducted eye, any observable strabismus caused by a paralyzed
oblique muscle will get worse when the affected eye is adducted, and the strabismus is likely to go away when
the affected eye is abducted. In our example of a paralyzed SO, any hypertropia will become
worse when the affected eye looks medially, whereas it may virtually disappear when the affected
eye abducts. By similar reasoning, since the superior and inferior recti play a dominant role in
determining the vertical position of an abducted eye, but a much smaller role in determining the
vertical position of an adducted eye, any observable strabismus caused by a paralyzed vertical rectus
muscle will get worse when the affected eye is abducted, and will diminish or go away when the
affected eye is adducted.
With only weakness (paresis) of a muscle, strabismus and diplopia may not be noticeable
until the patient actually attempts to move the affected eye in a direction that requires extra effort
by the weak muscle. For example, weakness of the SO may lead to a noticeable strabismus only
upon looking downward, or downward and inward. The chart on page 111 indicates the motions
of the eye that should be elicited in order to look for strabismus resulting from a paretic
extraocular muscle. Bielschowsky Head-Tilt Test for Testing the Superior and Inferior Obliques
Testing for weakness of an oblique muscle by eliciting elevation and depression of the adducted eye may sometimes be unrevealing. This is so because the vertical recti contribute to elevation/depression of an eye
that is moderately adducted (and there are other complicated reasons relating to changes in the intact extraocular muscles
after one of their colleagues has been paralyzed for a long time). The best way to
examine the strength of the superior and inferior oblique muscles relies on understanding the
cyclorotation that normally occurs when someone laterally flexes his/her neck. You know that if you ask a
patient to tilt the head to the right, he or she will incycloduct the right eye and excycloduct the left eye. The incycloduction is brought about by the SO and SR, the excycloduction by the IO and IR. If a person performing a head tilt to the
right has a weak right SO, the depressor action of that SO will be unable to counteract the elevating action
of the normal right SR. Hence, the right eye will deviate upwards during the head tilt. Similar reasoning reveals that if a patient had a weak left IO, its elevation action would not be able to overcome the depressor action of the left IR, and the left eye would move downward during the head tilt to the right. A head-tilt to the left serves to test the left SO and right IO.
The attempt to observe abnormal vertical deviation of an eye during head-tilts is called the
Bielschowsky Head-Tilt Test. Although logic would suggest that weakness of a vertical rectus
muscle could be revealed by this test (e.g., upon a head-tilt to the right, a weak right SR should lead to depression of the eye
by a normal SO), it has been observed that strabismus upon head-tilt is a consistent
observation when an oblique muscle is weak, but inconsistently present in the case of weak
vertical recti. This is probably related to the fact that the obliques are predominantly cyclorotators
when the eye is the primary position. Head Posture With Strabismus
In strabismus, the two optic axes fail to converge on the object being looked at. However, in some cases it may be possible for the patient to get the optic axes to point in the same direction by adopting a head position
that calls upon the good eye to point in the same direction as the affected eye. One example is
illustrated in Core Concept 70: if a lateral rectus is paralyzed and, as a consequence, the affected eye is adducted, the patient can get both optic axes to
point in the same direction by adopting a head position that calls upon the normal eye to abduct.
Paralysis of one or the other oblique muscles is frequently associated with an abnormal head
position. Since, in the primary position of the eye, these muscles are mainly cyclorotators, the
paralysis of either one causes a cyclodeviation (torsion) of the affected eye producing a peculiar
kind of strabismus called cyclotropia. Paralysis of the SO leads to an excyclodeviation
(excyclotropia) of the affected eye; paralysis of the IO leads to an incyclodeviation
(incyclotropia) of the affected eye.
Take the case of a patient who has an excyclotropia of the right eye due to SO
paralysis. She can avoid diplopia by adopting a head position in which excycloduction of
the right eye would normally occur, i.e., one in which the head is tilted to the left (see image below on the left). Such a position
induces the unaffected left eye to incycloduct, resulting in comparable torsions of the two eyes and
corresponding positions of their retinal images. (By the way, a head-tilt to the left will mask any right hypertropia seen with right SO paralysis. The patient "chose" this head position precisely because it does not require use of the right eye's incycloductors, including the SR that causes the hypertropia.) Head-tilts used to avoid diplopia
are referred to as ocular torticollis.

If you see a person with left torticollis that you believe might be ocular in origin, say to yourself "This person chose to have an excycloducted right eye and an incycloducted left eye." Therefore, they must have either a weak right SO or a weak left IO. Do other tests to determine which is the case. If you see a person with a right torticollis that you believe might be ocular in origin, say to yourself "This person chose to have an excycloducted left eye and an incycloducted right eye. Therefore, they must have either a weak left SO or a weak right IO. Again, do other tests to determine which is the case.
Check Ligaments
In the words of von Noorden (1990, Binocular Vision and Ocular Motility, 4th ed.,
CV Mosby, St. Louis), "there are numerous extensions from all the sheaths of the extraocular
muscles, which form an intricate system of fibrous attachments interconnecting the muscles,
attaching them to the orbit, supporting the globe, and checking the ocular movements." This
intricate system is thought to prevent certain muscles from overshortening, to support the eyeball
against the pull of gravity, and to keep the eyeball from being pulled backward into the depth of
the orbit by contraction of the rectus muscles. It is said that developmental anomalies of the
fascial system are more common than those of the extraocular muscles and are clinically more
significant. Thus, ophthalmologists put a lot of effort into naming and describing various parts of
the fascial system. If that becomes your chosen field, be forewarned.
Vomeronasal Organ, Vomeronasal Nerve (?), and the Nervus Terminalis (Cranial Nerve 0)
What I am about to discuss doesn't actually constitute a "Clinical Sidelight", but it's so interesting
I wanted to include it anyway. It
has now been demonstrated conclusively that adult humans possess a
vomeronasal
organ (VNO), once thought to have been lost during higher primate
evolution. The VNO is present bilaterally as a small epithelial tubular sac lying submucosally in
the antero-inferior part of the nasal septum. Each VNO has a tiny opening into the antero-inferior
region of the nasal cavity. In many mammals, a subpopulation of cells within the VNO are
chemoreceptive neurons that respond to stimulation by pheromones. These cells give rise to
axons that form a few vomeronasal nerves, which travel up the nasal septum and through the
cribriform plate to synapse on an accessory
olfactory bulb next to the main one. Human adults do not have an accessory olfactory bulb.
Furthermore, most researchers have not been able to find chemosensory cells in the human VNO, nor have
vomeronasal nerves been found in adult humans (Bhatnagar KP, Smith TD. 2001 The human vomeronasal
organ. III. Postnatal development from infancy to the ninth decade. J Anat 199:289-302; Witt M
et al. 2002 On the chemosensory nature of the vomeronasal epithelium in adult humans.
Histochem Cell Biol 117:493-509). Genes that in other mammals produce receptor molecules for
the chemosensory cells of the VNO are almost entirely nonfunctional in humans (Mombaerts P.
2004 Genes and ligands for odorant, vomeronasal and taste receptors. Nature Reviews
Neuroscience 5:263-278). Still, it must be said that some researchers believe the human VNO is
a functioning pheromone sensitive organ that communicates with the brain via vomeronasal
nerves (see Monti-Bloch L, et al. 1998 The human vomeronasal system. A review. Ann
NY Acad Sci 855:373-389).
A different set of axons beginning in the vicinity of the VNO (and also a nearby area of
the nasal septum mucosa) collect into a few nerve bundles that constitute the nervus
terminalis, another structure once thought to be
absent in adult humans. The bundles of the nervus terminalis course up the nasal
septum
and through the cribriform plate, but then pass along the medial aspect of the
olfactory
bulb and olfactory tract into the brain (Fuller GN, Burger PC. 1990 Nervus terminalis (cranial
nerve zero) in the adult human. Clin Neuropath 9:279-283). The cell bodies of these axons are
scattered along their
path to the brain. They are immunoreactive for luteinizing hormone releasing hormone (LHRH),
and in development some cells from the same embryologic source migrate along the nervus
terminalis into the hypothalamus to become the cells that secrete LHRH. Aside from playing the role of a "highway" in development, the function of the human nervus terminalis is unknown
(Schwanzel-Fukuda M, Pfaff DW. 2003 The structure and function of the nervus terminalis. Pp.
1001-1026 in Handbook of Olfaction and Gustation, RL Doty, ed., Marcel Dekker, NY).
Sinusitis
Because the ostia (i.e., openings) of the paranasal sinuses into the nasal cavities are small and
surrounded by easily swollen mucous membrane, the flow of air between the paranasal sinuses
and nasal cavity is highly restricted. Mucous secreted by the epithelium lining each sinus
normally flows into the nasal cavity unless the mucous membrane lining its ostium becomes
swollen to the point of occlusion. Then the patient will want to take decongestants to reduce this
swelling, open the ostium, and thereby "decompress" the sinus. Infectious organisms may pass
from the nasal cavity into the sinuses, leading to the well-known condition of sinusitis.
Genioglossus and Sleep
It has been suggested that some persons are subject to respiratory distress during sleep (sleep apnea)
because they have periods of inactivity of the genioglossus, with the result that the tongue falls
backward into the oropharynx. Certainly during general anesthesia, one must guard against the
tongue falling backward and obstructing the air passageway.
Lingual Frenulum
One cause of speech impediments is a short lingual frenulum, which may then be incised.
The dilator tubae portion of the tensor veli palatini is often called into action by the same
behaviors that require the rest of the muscle to tighten the soft palate. Thus, during the descent of
an airplane, passengers are advised to swallow or yawn (behaviors that induce soft palate tightening)in order to equalize pressure between the
external environment and middle ear cavity. These maneuvers often fail to work, indicating that
it is possible to contract the bulk of the tensor veli palatini without simultaneous recruitment of
dilator tubae. Eventually, however, a reflex swallow or yawn occurs in which the auditory tube is
opened.
It is branches of the central artery of the retina, and tributaries of the central vein, that are seen when looking into the eye with an ophthalmoscope.
Olfactory Nerve
In a routine neurologic examination, olfaction is tested with the simple goal of determining if the ability to smell through one nostril is the same as the ability to smell through the other nostril, i.e., to determine if there has been unilateral damage to the olfactory pathway. A nonirritating
odoriferous substance is placed beneath one nostril while the other nostril is compressed. The patient is asked if an odor is detected, and to identify it. Coffee, oil of peppermint, wintergreen, cloves, or camphor are commonly used. The test is then repeated on the other side. A difference between sides raises the suspicion of a tumor (e.g., a meningioma) compressing the olfactory bulb or tract on the side with the poorer sense of smell. This is a treatable condition. A fracture through one cribriform plate that damages fila olfactoria will also produce unilateral impairment of smell, but this is not treatable.
With the exception noted below, the observation that a patient has bilateral impairment of olfaction is not very significant. Some people are born with no ability to smell (anosmia). In people born with normal olfaction, the ability to detect odors declines past middle age (i.e., odor thresholds progessively rise in old people). Common nasal infections can lead to temporary (or more rarely, permanent) loss of smell, as can exposure to toxic chemicals. Blows to the front or back of the head that cause large anteroposterior excursions of the brain can lead to shearing off of the fila olfactoria as they pass through holes in the cribriform plate on their way to the olfactory bulb. If all the fila are torn, the result will be untreatable anosmia.
The important exceptions to the insignificance of bilateral olfactory impairment are patients with Alzheimer's disease or Parkinson's disease. Alzheimer's patients have unusually high odor thresholds for their age, and they suffer an even more dramatic reduction in their ability to identify and discriminate different odors. Patients with Parkinson's disease also experience olfactory deficits, but their impairment in odor identification is less severe, and their impairment in odor detection is more severe, than in Alzheimer's patients (Rahayel S et al. 2012 The effect of Alzheimer's disease and Parkinson's disease on olfaction: a meta-analysis. Behavioural Brain Res 231:60-74). There is evidence that the olfactory deficits in Alzheimer's disease precede the cognitive impairment, and that that the olfactory deficits in Parkinson's disease precede motor impairment. One may get information about the course of one these diseases by using sophisticated tests of odor detection, identification, and discrimination. Patients in the early stages of either disease, but with severe olfactory impairment, have a poorer prognosis. (I wish to acknowledge Chelsea Dahl, a Stony Brook medical student, for alerting me to the impairment of olfaction occuring in Alzheimer's and Parkinson's diseases, and to the role of olfactory assessment in predicting the courses of these diseases.)
Testing the Optic Nerve
Neuro-ophthalmologists have ways of accurately assessing visual field defects. In the more
typical physical exam, the exploration of visual fields is usually done simply by bringing a
wiggling finger into view of the patient from the sides, from above, and from below. The patient
looks straight ahead and is requested to state when the finger can first be seen.
Routine testing of extraocular muscles involves asking the patient to look at your finger as
you move it in directions that should elicit adduction and abduction of the eye, elevation and
depression of the eye when it is adducted, and elevation and depression of the eye when it is
abducted. Core Concept 62 discusses which muscles (and therefore which nerves) are required for
these motions. The clinical comments for Core Concept 62 provide additional information on
testing extraocular muscles. Test of the levator palpebrae superioris is as simple as asking the
patient to look upward so you can observe if elevation of the eyelid accompanies this effort.
Testing the parasympathetic pathway to the constrictor pupillae is done by shining a light in the
patient's eye. The pupil should constrict. Note that this pupillary light reflex is consensual, which
means that shining a light into only one eye causes both pupils to constrict. Testing the
sympathetic pathway to the dilator pupillae is done by shielding an eye from light; its pupil
should dilate. This reflex is also consensual.
A second test for the parasympathetic pathway to the constrictor pupillae relies on the accommodation reflex
that causes the pupil to constrict when one attempts to focus on an object very close to the eye.
Normally this involves convergence of the eyes, i.e., rotation so that their optic axes converge
on a nearby point. The test is performed by asking the patient to follow your finger as you bring
it toward the bridge of his/her nose. One assumes that the ciliary muscle is also contracting, but
there is no easy way of determining this. Paralysis of the ciliary muscle should cause focusing
problems, but these may be unnoticed by the patient.
While damage to the oculomotor nerve affects both the pupillary light and pupillary
accommodation reflexes, some central nervous system diseases (e.g., neurosyphilis) produce a
pupil that constricts on accommodation but not in response to light. This is called an
Argyll-Robertson pupil (mnemonic: the initials AR correspond to Accommodation Reactive).
Isolated lesions of the trochlear nerve are uncommon. The abducens is the most frequently
damaged of all nerves feeding extraocular muscles. It is the first nerve to be affected by septic
thrombosis of the cavernous sinus. Aneurysm of the internal carotid artery within the cavernous
sinus may put pressure on the abducens. A variety of tumors at the base of the brain will tend to
compress the nerve against the clivus.
The Swinging Flashlight Test
This is really a test to discover if one of a patient's eyes has a diminished ability to perceive light (by virtue of a retinal disease) or has a diminished ability to tell the brain it has perceived light (by virtue of an optic nerve disease). Although the swinging flashlight test is a test of retinal or optic nerve function, it cannot be understood until one has a knowledge of the pupillary light reflex, so I am presenting it here.
If you shine a light in one eye, hold it there for about a second to allow the pupils to constrict, then quickly move the light to the other eye and hold it there for about a second, there are three possible outcomes.
(a) If both eyes are equal in their ability perceive the light and transmit this information to the brain, there will be no change in pupil size as the light impacts on the second eye. Both pupils will maintain the same degree of constriction as they had acquired when the light was shown in the first eye.
(b) If the second eye perceives the light as dimmer than did the first eye, or cannot fully transmit its information to the brain, then both pupils will dilate even as the light is shown in the second eye. They will dilate until the pupil of the second eye reaches the size appropriate for the amount of light the brain believes is being shown to that eye. This second eye is said to have a relative afferent pupillary defect (RAPD).
(c) If the second eye perceives the light as brighter than did the first eye (because the first eye has retinal disease), or more fully transmits its information to the brain (because the first eye has optic nerve disease), then both pupils will constrict further as the light is shown in the second eye. They will constrict until the pupil of the second eye reaches the size appropriate for the amount of light the brain believes is being shown to that eye.
Hence, by swinging a light back and forth between the eyes, holding it in front of each for about a second, you will be able to get information about differences between the eyes in optic nerve or retinal functioning. If the pupils do not change in size after a swing, then both eyes are operating at the same level. If the pupils dilate after a swing, then the second eye is functioning more poorly; if both eyes constrict after the swing, then the second eye is functioning better. (Obviously, the swinging flashlight test only works if there is no oculomotor nerve disease, and it cannot reveal instances of disease that affects both optic nerves or both retinas equally.)
Click here to see the swinging flashlight test in action. What this video shows is a swinging flashlight test performed on a patient with left optic neuritis. Using increasingly dark filters, the physician will attempt to find out how much light must be stopped from reaching the right eye in order to make it as "bad" as the left eye. He will have succeeded when the pupils of the eyes no longer change size as light is swung between them.
Core Concept 71 lists some symptoms of trigeminal palsy. No mention was made of problems
arising from paralysis of nonmasticatory muscles innervated by the trigeminal. That's because I
have not encountered a description of middle ear problems in adult humans arising from paralysis of the tensor veli palatini, nor have I discovered reports of difficulties in swallowing resulting from paralysis of the mylohyoid or of auditory symptoms resulting from paralysis of the tensor tympani.
For your information, extirpation of the
tensor veli palatini in experimental animals does lead to severe middle ear pressure dysfunction. Also, human children born with cleft palate almost always accumulate fluid in the middle ear cavity, which interferes with their hearing and frequently leads to middle ear infections. The most commonly accepted explanation is that cleft of the soft palate, by removing the fixed point of insertion of the tensor veli palatini, greatly diminishes the ability of this muscle to open the Eustachian tube. This is treated by placing a tiny drainage tube ("myringotomy tube") through the eardrum. Interestingly, even in children whose cleft palate is not repaired, middle ear problems tend to get better by age 3 or 4, probably because the Eustachian tube inclines a bit downward as one matures. (I wish to acknowledge Dr. Alexander Dagum, Chief of Plastic Surgery at Stony Brook University, for this information.)
Testing the Trigeminal Nerve
Damage to the ophthalmic nerve is tested by determining the responsiveness of the skin of
the forehead (frontal nerve) to touch and prick with a sharp object (like a broken Q-tip). A
second test involves the corneal reflex. When the cornea is touched, the sensation travels via
V1 back to the trigeminal nerve and thence to the brain. Here fibers synapse with facial
neurons innervating the palpebral portion of orbicularis oculi, which is caused to contract,
producing a blink. Like the pupillary light reflex, the corneal reflex is consensual, i.e., both
eyelids blink when either cornea is touched. Obviously, disturbances of the corneal reflex will
occur if either the sensory or motor limb is damaged. If the sensory limb is damaged, neither
eyelid will blink when the affected cornea is touched. On the other hand, if touching the cornea
of one eye produces a blink in the opposite eye, the examiner knows that V1 is working
and that the defect is in the ipsilateral facial nerve.
Damage to the maxillary nerve is usually tested only by assessing the responsiveness of the
skin over the front of the cheek (infraorbital nerve) to touch and pain. Nasal, palatal, and upper
dental sensation are affected by damage to maxillary nerve, but these are not tested for routinely.
During a routine exam, the test for sensory fibers that run in V3 is usually confined to
the skin over the chin (mental nerve) and side of the cheek (buccal nerve). General sensation to
the front of the tongue (lingual nerve) may also be tested. Obviously, a thorough neurological
exam can involve tests over other regions (e.g., temple, upper part of external ear).
Tests for strength of the masseter and pterygoids are often made in routine physical
examinations. The examiner places one hand over the left masseter and the other hand over the
right masseter, and then asks the patient to clench his or her teeth. An assessment is made about
the degree to which one side may be contracting less strongly than the other. (The test can also be
done with the hands placed over the temporalis muscles, but these are less easily palpable.) The
lateral pterygoid, medial pterygoid, and superficial masseter, when acting together on one side,
protract that side of the mandible and cause the chin to deviate toward the opposite side. The left protractors push
the chin toward the right; the right protractors push the chin to the left. If the examiner places a
hand on the right side of the chin and attempts to push the jaw to the left, the patient must use the
left protractors to resist this. If the examiner places a hand on the left side of the chin and
attempts to push the jaw to the right, the right muscles must be used to resist this. By asking the
patient to resist such pushes on the jaw, an assessment of strength of the jaw protractors on one
side compared with those on the other may be made.
The symptoms of damage to the facial nerve within the posterior wall of the tympanic cavity
are summarized in Core Concept 72. Additionally, some patients with damage to the chorda tympani
also complain of partial numbness of the tongue on the ipsilateral side. It is not known whether
this is simply the way persons perceive disruption of sensory input for taste from the tongue, or if some of
the sensory axons within the chorda tympani of humans are connected to mechanoreceptors, as
occurs in cats.
Surgery on the middle ear may damage the facial nerve within the labyrinthine wall of the
tympanic cavity, leading to all the symptoms mentioned in Core Concept 72. Tumors within the
petrous temporal may affect the facial nerve at the site of the geniculate ganglion. This leads to the symptoms mentioned in Core Concept 72, plus loss of tearing on the affected side. Lesions of the facial
nerve between the brain and the facial canal may affect one root and not the other, because the
two roots are actually separate during this part of their courses.
There is a peculiarity about the cortical input to the facial nuclei of the brainstem that is
useful in diagnostics. You will learn in neuroanatomy that, in general, a cerebral hemisphere controls muscles on the contralateral side of the body.
As one would expect, the facial motoneurons projecting to the lower two thirds of the face receive cortical input only from the opposite
cerebral hemisphere. Surprisingly, however, facial motoneurons going to the upper third of the face receive
cortical control from both the right and left cerebral hemispheres. Thus, if there is a unilateral interruption of the pathway from the cerebral cortex to the brainstem, paralysis of the opposite side's mouth and cheek muscles will be
will be full-blown, but the orbicularis oculi and frontalis of that side will still be able to weakly contract.
Testing the Facial Nerve
Testing the facial nerve during a routine physical examination begins with observing the
appearance of the face to assess the normality of skin creases, width of the palpebral fissures, and
position of the corners of the mouth. Then, the patient is asked to raise the eyebrows or wrinkle
the forehead (frontalis) and the examiner looks to see if this is done symmetrically. The patient
may be asked to close the eyes very tightly (orbicularis oculi) and the examiner tries to pry them
open by pushing up on the eyebrows. A broad smile is requested (several muscles) and assessed
for symmetry. The patient is asked to puff out the cheeks. Puffing out one's cheeks is made
possible by the action of orbicularis oris to prevent escape of air between the lips. If one side
is very weak, air escapes on that side. If air does not escape, the examiner may apply a test of
strength by pushing in on both cheeks to see if the orbicularis oris on one side can be
overwhelmed.
Only if these tests of facial muscles reveal a deficit does the examination progress to a test of
taste or lacrimation. Taste on the anterior two thirds of the tongue can be evaluated by applying a
strong tasting solution (e.g., salt, sugar, citric acid, quinine) to its right and left edges, where most
of the taste buds are concentrated. There exist special absorbent paper strips that can be applied
to the surface of the eye for assessing tear production.
Vestibulocochlear Nerve
The assessment of the sense of equilibrium, or of auditory sensitivity by sound frequency, is left to
specialists. However, a routine physical examination may attempt to judge general hearing
acuity, particularly as it depends on adequate operation of the middle ear mechanism.
A first test - the Weber test - can be done to determine if there is unilateral hearing
diminution due either to sensorineural (cochlea or nerve) or conductive (eardrum and ossicular
chain) problems. The stem of a vibrating tuning fork (256 or 512 Hz) is placed in
contact with the vertex of the skull so that sound is sent directly through the bone to reach both
the right and left cochleae. If hearing is normal, the sound will be reported as being equally loud
in both ears. As you might expect, if a cochlea or its nerve is damaged on one side, the sound of
the tuning fork will be heard as louder on the opposite, normal side. On the other hand, you
might be surprised to learn that if there is a problem on one side with the conductive mechanism,
the tuning fork will actually be heard as louder on that abnormal side. This is because the sound
of the tuning fork transmitted through the bone of the skull competes with room noise
transmitted through the eardrum and ossicular chain. Such room noise becomes a poorer
competitor if the conductive mechanism that brings it to the cochlea is defective, with the
consequence that the tuning fork sounds louder in that ear. To summarize, in a Weber test,
lateralization of the tuning fork's sound to a particular side occurs if there is a problem either
with that side's conductive mechanism or the opposite side's sensorineural mechanism. The
inherent ambiguity of this result should be resolved by the application of the Rinne test,
described below.
Although the Weber test is described in most physical diagnosis and neurology
texts, there is evidence that it has a high risk both of giving false positive and false negative
results (Miltenburg, DM, J. Otolaryngology, 23:254-259, 1994). My neurology colleagues don't use it.
They simply whisper a number into one ear while rubbing their thumb and fingers next to the opposite ear so as to shield it from hearing the whispered number. They repeat this on the opposite side. If the patient can identify a whispered sound equally well in both ears, then he or she is considered to have acceptable hearing.
If a patient has an abnormal Weber test, or can't hear a whispered sound, the Rinne test is considered a pretty good
(though not perfect) method for
determining if the hearing loss is due to a conductive or sensorineural problem. The
Rinne test is applied to each side separately. Various neurology and physical diagnosis texts
describe it as consisting of three steps: (1) apply the stem of a vibrating tuning fork to the
patient's mastoid process so that the vibrations reach the cochlea via bone conduction, (2) ask the
patient to report when the sound is no longer heard, (3) then place the tines of the tuning fork
near the external auditory meatus and inquire if the sound can once again be heard. If the patient's
middle ear on the tested side is operating normally, the sound will once again be heard, usually
for an additional period of time that equals the duration of the audible bone conduction through
the mastoid process.
Otolaryngologists seem to agree that the accuracy of the Rinne test can be improved by
performing it somewhat differently than just described. They recommend the following
method: Glossopharyngeal Nerve
The routine test of glossopharyngeal function is the gag reflex. This reflex consists of
pharyngeal constriction when the back wall of oropharynx is touched. The glossopharyngeal
nerve is supposed to be the sensory limb of the gag reflex; the vagus is the motor limb. However,
since some authors state that the gag reflex is not lost after glossopharyngeal nerve section, the vagus
may participate in conducting pharyngeal sensation. If this is true, then the standard test for
glossopharyngeal function is not informative.
Taste on the posterior third of the tongue can be assessed by applying a small electrical
current between copper electrodes placed on the back of the tongue. An acid or metallic taste is
elicited. This is not a common procedure. Applying solutions of strong taste to the back of the
tongue is not a good method because of the rapid spread of the solution to the other side. Another reason not to bother with such a test is that some
authors report that intracranial transection of the glossopharyngeal nerve does not lead to loss of
taste or general sensation from the tongue. It would seem that more remains to be learned about
the complete pathway of such modalities. Frey's Syndrome
As you know, the glossopharyngeal nerve carries the preganglionic parasympathetic axons responsible for stimulating salivary secretion by the parotid gland. These axons synapse on cells of the otic ganglion, whose postganglionic axons travel through the auriculotemporal nerve to reach the gland. Partial or total parotidectomy is a treatment for parotid tumors (which fortunately are usually benign). Several months (sometimes longer) following such surgery, when patients are eating they often experience sweating in the skin over the site of removed glandular tissue. Gustatory sweating (i.e, sweating that occurs when you taste something) arising as a consequence of parotid injury is called Frey's syndrome. It is sometimes accompanied by facial flushing in the same region. Frey's syndrome is thought to arise when transected postganglionic parasympathetic axons grow into the skin and aberrantly innervate sweat glands and blood vessels. Some surgeons try to prevent the development of Frey's syndrome by interposing a barrier between the cut surface of the parotid tissue and the undersurface of the skin. Flaps from the sternocleidomastoid, SMAS, temporoparietal fascia, or vascularized fat have been used. So has acellular dermis that can be purchased commercially. These barriers may also reduce the sunken appearance of the face that would otherwise occur at the site of the removed parotid tissue. However, their success in preventing Frey's syndrome is debated (Witt RL, Pribitkin EA. 2013 How can Frey's Syndrome be prevented or treated following parotid surgery? Laryngoscope 123:1573-1574). What appears to be most successful in treating Frey's syndrome is intradermal injection of botulinum toxin, which usually has a beneficial effect that lasts well past the time when the physiological action of the toxin has dissipated. It can also be repeated if necessary.
1) strike a 256 or 512 Hz tuning fork and hold its tines about one inch from the
external auditory meatus for a few seconds;
2) move the stem of the tuning fork onto the
patients mastoid process for a few seconds;
3) ask the patient whether the sound was
louder in the front or the back.
If the patient reports that the front (i.e., air conduction)
sounded louder than the back (i.e., bone conduction), the test indicates that nothing is wrong with
the conductive mechanism and that any hearing loss is probably sensorineural in origin. If the bone
conduction sounded louder than the air conduction, there is a significant likelihood of a problem
with the conductive mechanism. The Rinne test is not considered very useful as a general screening tool for hearing loss because a normal test is often found in people with hearing impairment (Bagai A, Thavendiranathan P, Detsky AS. 2006 Does this patient have hearing impairment? JAMA 295:416-428.).
Vagus Nerve
Core Concept 74 of the first edition presents a discussion of how vocal fold position
following injury to the recurrent laryngeal nerve (RLN) will be different from vocal fold position following injury to the vagus proximal to its
superior laryngeal (SL) branch. That discussion was based on the Wagner-Grossman hypothesis, which had nearly
universal acceptance prior to 1993. Since that time (and largely initiated by the research of Dr.
Gayle E. Woodson, Southern Illinois University School of Medicine) evidence has accumulated
that no such difference exists. The second edition of Core Concepts reflects the current view, but I will discuss it in a bit more detail here.
First and foremost, it seems that except under the experimental circumstance of electrically induced maximum contraction, the cricothyroid muscle does not produce vocal fold adduction. Consequently, even though the cricothyroid muscle remains intact after complete injury to an RLN, the affected vocal fold does not immediately assume a taut paramedian position. Instead, immediately after complete injury to an RLN, the ipsilateral vocal fold is flaccid and lies the intermediate position. The symptoms associated
with such a paralyzed vocal fold are (1) hoarse and breathy voice (dysphonia), (2) weak cough, (3) risk of
aspiration of fluids (which risk arises not only because the folds cannot be tightly approximated
but also because sensation is diminished on one side of the glottis), and (4) exertional dyspnea
(breathing during normal activities is not a problem since the intact cord can compensate for the
mildly narrowed glottis by wider abduction; only during exertion is there likely to be any
difficulty breathing). If the vagus is injured proximal to its SL branch, the
ipsilateral vocal fold appears the same as just described for an RLN injury. In other words, one
cannot diagnose the site of nerve injury based on vocal fold position.
Regardless of the site of nerve injury, after several months the paralyzed vocal fold may
move
medially, sometimes actually reaching the paramedian position. This is the usual occurrence in cases of RLN injury. One explanation offered for why
a paralyzed vocal fold might move medially is reinnervation by axonal regrowth from the part of
the nerve proximal to the injury. Animal experiments have demonstrated a remarkable ability of
RLN axons to cross surgically created gaps in the nerve and eventually reach the internal
laryngeal muscles on the affected side. The axons do not end up going to the same muscles they
had originally innervated, so useful control of the reinnervated vocal fold is not regained. However, since
there are four times as many adductor muscle motor units as posterior cricoarytenoid motor units,
the statistically favored effect is to cause a more adducted position of the cord. Additionally,
reinnervation of the thyroarytenoid muscle reverses atrophy of this muscle and leads to increased
bulk of the paralyzed fold. As a result, there is a diminution of symptoms, because the intact fold is now better able to make firm contact with the
fuller, tauter paralyzed fold.
By itself, reinnervation does not always happen. Consequently, one approach to treating unilateral vocal fold paralysis caused by nerve injury is to surgically anastomose one of the major branches of the ansa cervicalis to the distal stump of the RLN (reviewed in Paniello RC. 2004 Laryngeal reinnervation. Otolaryngol Clin N Am 37:161-181), or to the branch of the RLN that goes to the adductor muscles (Zheng H et al. 1996 Update: laryngeal reinnervation for unilateral vocal cord paralysis with the ansa cervicalis. Laryngoscope 106:1522-1527). This results in partial denervation of the infrahyoid strap muscles, but the loss is barely noticeable. There has also been a study in which the hypoglossal nerve was cut and then anastomosed to the distal part of the RLN. As stated on p. 133 of Core Concepts, speech, chewing, and swallowing are affected only slightly when half the tongue is denervated. If the surgeon opts against reinnervation of the laryngeal muscles, or if the procedure fails to produce the desired result, other surgical treatments to "medialize" the paralyzed fold can be attempted. [I want to acknowledge Wai Lee, a Stony Brook medical student, for bringing the technique of laryngeal reinnervation to my attention.]
Bilateral RLN injury requires the patient to be intubated. This is not because the two vocal folds are fixed in the paramedian position (although this may happen with time). Intubation is required because air moving past the flaccid vocal folds experiences a pressure drop (due to Bernoulli's Principle) that causes them to be "sucked" closer together. Thus, the airway becomes compromised on any but the slowest inspirations. (I thank my colleague Dr. Ghassan Samara, Dept. of Surgery, Stony Brook University, for this tidbit.)
Testing the Vagus Nerve
If the patient presents no symptoms attributable to vagal damage, routine testing of the vagus nerve
consists of observing of the soft palate at rest and while the patient says "Ah". If the soft palate droops on one side, or it does not rise on one side
when the patient says "Ah", paralysis of the levator veli palatini is indicated and damage to the ipsilateral vagus must be suspected. Failure of the
paralyzed half of the palate to rise when the patient says "Ah" may cause the uvula to shift to
the intact side, and this might be easier to assess than how high the soft palate rises. The gag reflex may also be elicited to test for the vagus. If the contraction of the pharynx that is elicited by touching its back wall is absent
on the same side as the drooping soft palate, this is further indication of vagal malfunction.
Anesthesia of the Airway for
Orotracheal Intubation in a Conscious Patient (I want to
acknowledge Dr. Michael M. Todd, Professor of Anesthesiology, University of Iowa, for
assistance with this topic.)
Whereas many patients are given intravenous anesthesia prior to airway intubation, selected
patients (e.g., those with cervical spine fractures) are intubated while awake. It is then necessary
to anesthetize the oropharynx and larynx to provide comfort and eliminate the risk of injury
associated with coughing and gagging. A solution of lidocaine sprayed into the back of the mouth
is often sufficient for oropharyngeal anesthesia, but this may be supplemented with an injection
of lidocaine into the middle of the palatopharyngeal fold (posterior faucial pillar), where it will
block the glossopharyngeal nerve prior to its branches to the tongue and adjacent region of the
pharynx. Anesthesia of the larynx is accomplished using two approaches. Sensation from the
supraglottic larynx is eliminated by administering lidocaine adjacent to the internal laryngeal
nerve (although this technique is usually referred to as "superior laryngeal nerve block"). It will
be recalled that the internal laryngeal nerve enters the larynx by piercing the posterior portion of
the thyrohyoid membrane. Thus, one may either aim the needle to hit the greater cornu of the
hyoid bone just anterior to its tip, then inject anesthesia as you walk the needle inferiorly, or one
may aim for the superior border of the thyroid lamina in front of its superior horn and inject
anesthesia as you walk the needle upward. In either case, the needle is also pushed through the
thyrohyoid membrane (which offers a palpable resistance) and anesthetic solution injected
around the nerve deep to this structure. The lower part of the larynx is made insensate by
spraying lidocaine through a catheter that has been inserted either through the median
cricothyroid ligament or through the trachea above or below the first tracheal ring. Testing the Accessory Nerve
Assessing the strength of the sternocleidomastoid and trapezius is done as a part of any
routine test for the integrity of the accessory nerve. The patient is asked to turn the head to one
side against resistance from the examiner. A resisted turn to the right tests the left
sternocleidomastoid,
and vice versa. Again, the examiner is trying to discover weakness of one side relative to the
other. Another way to judge strength of the sternocleidomastoids is to have the patient attempt to
flex the neck against resistance applied to the forehead. In this case, the examiner compares
strength of the right and left muscles by palpating the rigidity of each tendon that comes from the
manubrium.
To test for strength of the trapezius, the patient is asked to shrug the shoulders against
resistance by the examiner. Both sides are tested simultaneously so that a weakness of one side
relative to the other can be detected. Clearly this test informs one only about strength of the upper
fibers of the muscle, but these are the ones that receive most of their innervation from the
accessory nerve.
Cerebral control of the sternocleidomastoids is unusual. Whereas the general rule is that one
side of the cerebral cortex controls muscles on the opposite side of the body (but see discussion
of superior facial muscles above), the sternocleidomastoids get cortical input from both cerebral
hemispheres. As would be predicted from the general rule, the contralateral hemisphere
stimulates the sternocleidomastoid when you use it to flex or laterally flex your neck. For
example, a right hemisphere lesion causes weakness in the left sternocleidomastoid that can be revealed when you try
to touch your left ear to your left shoulder. Unexpectedly, the ipsilateral hemisphere stimulates
the sternocleidomastoid when the muscle is used to turn the head. For example, when you want to turn your head
to the right, use of your left sternocleidomastoid is initiated by the left cerebral cortex.
Since the left cortex also causes your eyes to turn to the right, ipsilateral cerebral control of
sternocleidomastoid during head turning behaviors is functionally sound. Testing the Hypoglossal Nerve
Routine examination of the hypoglossal nerve consists of a request that the patient stick out
the tongue and wiggle it from side to side. In theory, the left genioglossus is
primarily responsible for shoving the tongue to the right, while the right genioglossus is chiefly
responsible for shoving the tongue to the left. If the tongue can only be wiggled to one side, the muscles of
that side are paralyzed. The patient may also be asked to push first one, and then the other, cheek
out with the tongue while the examiner resists the movement. Again, in theory, the left genioglossus is
primarily responsible for pushing out the right cheek while the right genioglossus is chiefly
responsible for pushing out the left cheek. This test is entirely analogous to resisting sideways
deviations of the chin in order to assess mandibular protractors.
Stimulation of the Hypoglossal Nerve to Treat Obstructive Sleep Apnea
It was mentioned in Core Concept 66 that the genioglossus, a protractor of the tongue, plays a significant role in keeping the airway open during both wakefulness and sleep. Persons with obstructive sleep apnea (OSA) have a problem keeping the airway open during sleep. The blockage occurs at the level of the oropharynx. The cause for this blockage is probably multifactorial, but it has been shown that in sleeping apneic patients, spontaneous prominent contractions of genioglossus are associated with moments of airway patency. The standard treatment for OSA is continuous positive airway pressure (CPAP), but some patients cannot tolerate this procedure, and others simply fail to adhere to its requirements. A new treatment for such patients entails stimulation of the nerve that supplies genioglossus timed to inspiratory efforts (Mauer JT et al. 2012 Operative technique of upper airway stimulation: an implantable treatment of obstructive sleep apnea. Oper Tech Otolaryngol 23:227-233). The hypoglossal nerve is identified in the digastric triangle as it passes onto the surface of the hyoglossus. The free posterior edge of mylohoid is retracted anteriorly, allowing the nerve to be followed forward. Before reaching the halfway point of its course across hyoglossus, the hypoglossal nerve gives off a branch to geniohyoid and one or more lateral branches that go to hyoglossus, styloglossus, and some intrinsic longitudinal muscles. After that, the continuation of the nerve is called its medial branch, which innervates genioglossus and the remaining intrinsic muscles. This medial branch is identified, a stimulating cuff placed around it, and the surgeon verifies that stimulation protrudes the tongue. The stimulating cuff is connected to an implantable pulse generator that also receives input from a small pressure-sensing device placed between the external and internal intercostal muscles of the 4th interspace. When this device senses that inspiration begins, it tells the pulse generator to stimulate the medial branch of the hypoglossal nerve. The patient turns the system on at bedtime, but leaves it off during wakefulness. The procedure is performed only on the right side, but a study of over 100 patients demonstrated that this method of treating OSA "resulted in significant and clinically meaningful reductions in the severity of obstructive sleep apnea" (Strollo PJ Jr et al. 2014 Upper-airway stimulation for Obstructive Sleep Apnea. N Engl J Med 370:139-149).
Parotid Gland
In surgery on the parotid gland, it is important to see the facial nerve so that it be preserved.
There are a variety of ways to locate it just below the stylomastoid foramen. One is to find the posterior belly of the digastric and trace this upward; the
facial nerve is anterior to it near the base of the skull. Sometimes surgeons find it the way we do in dissection. That is, they locate a small branch crossing the masseter and trace this proximally.
The skin incision for parotid surgery usually sacrifices the anterior branch of the great
auricular nerve.
Epistaxis
Nosebleeds (epistaxis) are classified as anterior or posterior. Anterior bleeds usually stop by
themselves; if not, packing is usually successful. Posterior bleeds are harder to control. If all
conservative measures fail, the surgeon enters the pterygopalatine fossa through the maxillary
sinus and ties off the inner division of the maxillary artery. A newer approach entails
catheterization and embolization of the sphenopalatine and descending palatine arteries under
radiographic guidance. However, regardless of the technique used to occlude the branches of the
maxillary artery to the nose, many surgeons recommend simultaneous ligation of the anterior
ethmoidal artery because it anastomoses with such branches. Even this procedure may fail and
posterior ethmoidal artery ligation also be necessary.
More on Horner's Syndrome
The mild ptosis of Horner's syndrome can be easily distinguished from the more marked
ptosis due to levator palpebrae superioris paralysis simply by asking the patient to direct the gaze
upward, which will elicit elevation of the upper lid if the LPS is intact.
One anatomically interesting phenomenon is the occurrence of a reversible Horner's
syndrome in some persons who experience migraine headaches. Regardless of what might trigger a migraine, the actual headache is believed to
be caused by vasodilation of meningeal branches of the external carotid artery. However, in some
persons the vasodilation may also involve the internal carotid artery. Since this vessel passes through
the inexpansible carotid canal of the petrous temporal, expansion of the ICA can compress and
temporarily damage the sympathetic nerves that surround it. The result is a partial Horner's syndrome (affecting the eye and forehead)
that resolves itself over the course of the next few months. Excessive Frequency and
Extent of Facial Blushing (I wish to thank Peter Yoo, a Stony Brook medical student, for
drawing my attention to this Clinical Sidelight.)
Some persons blush intensely at the slightest provocation. This can lead to dread of social situations and be psychologically debilitating. Since emotional
vasodilation of facial vessels is controlled by preganglionic sympathetic cells lying
predominantly in the T2 level of the spinal cord, interrupting the course of their axons can cure
the condition. Surgeons perform an endoscopic procedure in which the sympathetic trunk is cut just superior to the T2 ganglion, or the T2 ganglion (and sometimes also T3) may be removed entirely. This operation was initially developed to treat excess sweating in the palm, but a somewhat different technique is now recommended for that condition. Sympathicotomy (cutting the sympathetic trunk) or sympathectomy (excising a portion of the trunk) at the T2 level has also been used to treat complaints of excessive facial sweating.
Parotid Duct
The rule of thumb is that a vertical laceration of the face below the zygomatic arch and
posterior to the lateral canthus of the eye threatens the parotid duct. This is so because the duct
lies on the relatively unyielding masseter here.
Erb-Duchenne Syndrome
Falls that cause the head and shoulder to be pushed apart may result in tearing, or actual
avulsion from the spinal cord, of the upper roots (C5 and C6) of the brachial plexus. The same
damage may occur in a newborn if the person "assisting" a normal head-first delivery tries to
promote passage of the shoulders by laterally flexing the child's neck and pulling. The motor
symptoms of brachial plexus upper root damage are said to constitute the Erb-Duchenne
syndrome. Since these roots predominantly innervate muscles proximal to the elbow, motions at
the shoulder and elbow joints are most affected. There occurs paralysis of abduction and lateral
rotation of the upper arm, paralysis of elbow flexion, and weakness of supination of the forearm.
The upper limb hangs limply at the side with the upper arm in medial rotation and the forearm pronated
(the so-called waiter's tip position). There is also a characteristic sensory deficit
associated with injury to C5 and C6. As might be expected, the skin over the pre-axial side of
the limb is without feeling.
To a certain extent one can predict which muscles will be paralyzed in Erb-Duchenne
syndrome from a knowledge of brachial plexus formation and the distribution of specific nerves.
The upper roots form the superior trunk, which is the sole source of axons to the suprascapular
nerve. The superior and middle trunks (C5, C6, C7) are the sole source of axons to the lateral
cord, from which the musculocutaneous nerve is derived. Unfortunately, there are other paralyses
that cannot be deduced in this way.
Avulsion of C5 and C6 leads to paralysis of some trunk muscles attaching to the shoulder
girdle (e.g., subclavius, rhomboids, and most of serratus anterior). However, Erb-Duchenne
syndrome is defined by the consequences of limb muscle denervation and can occur by damage
to the superior trunk of the brachial plexus, which will not affect trunk muscles innervated by C5
and C6.
Klumpke Syndrome
Damage to the lower roots (C8 and T1) of the brachial plexus can occur during strong
upward traction on the upper limb. This might occur if a person attempts to stop a fall by
grabbing onto an overhead support. It also may occur during delivery of a neonate if an attempt is
made to facilitate passage of the trunk by pulling on the upper limb. The motor deficits that result
from damage to the lower roots of the brachial plexus constitute the Klumpke syndrome. Since
these roots innervate predominantly muscles distal to the elbow, motions of the wrist and hand
are most affected.
We can predict certain of the deficits in Klumpke syndrome by realizing that C8 and T1 are
the sole source of axons to the medial cord and ulnar nerve. Thus, all the ulnar innervated
muscles of the forearm and hand will be paralyzed. It just so happens that those axons of the
median nerve destined for intrinsic hand muscles and for the deep extrinsic digital flexors are
also derived from C8 and T1. The sensory deficit in Klumpke's syndrome is characterized by loss
of sensation in the skin along the postaxial aspect of the upper limb.
Anastomoses Between Median and Ulnar Nerves
The ventral division axons for muscles distal to the elbow are carried by either the median or
ulnar nerve. Interestingly, nerve fibers that normally run with the ulnar nerve may sometimes
leave the brachial plexus in the median nerve, and vice versa. Such fibers may stay with their
abnormal carrier all the way to the muscle for which they are destined, in which case that muscle
has an anomalous innervation from the "wrong" nerve. More frequently, these fibers cross from
the abnormal carrier to their proper carrier somewhere below the elbow. The most common form
of such a median/ulnar communication is called the Martin-Gruber anastomosis, which occurs in
about 15% of limbs. It arises when motor axons that should have left the brachial plexus with the
ulnar nerve to innervate certain muscles of the hand, instead leave with the median nerve. Then
in the forearm, these misdirected axons correct their mistake by crossing from the median nerve
to join the ulnar nerve, thereby creating the anastomosis.
The significance of Martin-Gruber anastomosis is that injury to the median nerve proximal to
the anastomosis will lead to specific hand muscle paralyses expected from ulnar nerve damage,
and damage to the ulnar nerve proximal to the anastomosis fails to yield these expected
symptoms.
Sympathectomy (or Sympathicotomy, or Sympathetic Chain Clipping) for Palmar Hyperhidrosis
The upper limb receives its sympathetic innervation through
gray rami that join the ventral rami of the brachial plexus. The postganglionic axons in these gray rami come from cells in
the middle cervical sympathetic ganglion, the inferior cervical sympathetic ganglion, and the first thoracic ganglion. For many years people believed that these postganglionic cells are controlled by preganglionic axons that arise in the
T2-T3 spinal cord segments, travel in the 2nd and 3rd white rami communicantes to the T2 and T3
paravertebral ganglia, then ascend in the sympathetic chain to the ganglia of synapse. As a result,
surgical removal or destruction of the T2 and T3 sympathetic ganglia, or simply cutting the
sympathetic trunk (i.e., sympathicotomy) at one or more sites just below the T1 ganglion, became
an accepted procedure to treat a distressing condition in which the patient is plagued by excessive
sweating of the palm (i.e., palmar hyperhidrosis). As long as the T1 ganglion and its white ramus are left
unscathed, no ocular symptoms of a Horner's syndrome are produced. However,
since the sweat glands and vasculature of the face are innervated mainly by the T2 level of the spinal
cord, functions of these structures are affected by such surgery. Indeed, this surgery may be done as a means to treat excessive facial sweating or blushing .
Recently, it has been discovered that one can effectively treat palmar hyperhidrosis by interrupting the sympathetic trunk between the T3 and T4 ganglia (Lin CC & Telaranta T. 2001 Annales Chirurgiae et Gynaecologie 90:161-166). This means that the preganglionic cells for the upper limb reside predominantly in the T4 and lower (T5, T6?) segments of the intermediolateral column (although it does seem that T3 provides a small amount of sympathetic innervation to the palms.) Leaving the sympathetic trunk intact above the T4 ganglion has the distinct advantage of preserving the sympathetic input to the face. Also, this newer procedure is less often associated with excessive compensatory sweating elsewhere in the body, which is one of the most unpleasant side effects of transection of the sympathetic trunk above the T3 or T2 ganglia.
There are some people who experience hyperhidrosis of the armpit. If this occurs along with palmar hyperhidrosis, interrupting the sympathetic trunk just above the T4 ganglion is often effective in treating both conditions, although the success rate for eliminating the axillary hyperhidrosis is lower than that for eliminating the palmar hyperhidrosis (Neumayer C et al. 2005 Arch. Surg. 140:676-680). The fact that the axillary apocrine glands (which produce the odiferous secretion) are not under nervous control may account for the higher failure rate of sympathicotomy in treating axillary hyperhidrosis. I have read that if a person's sole complaint is axillary hyperhidrosis, interrupting the sympathetic trunk between T4 and T5 helps as much as interrupting it above T4. However, since surgery for this condition may or may not produce the desired result, and since it is possible to surgically remove the glands of the armpit without major disfigurement, some physicians do not recommend sympathicotomy if axillary hyperhidrosis is the sole complaint.
As an aside, some surgeons now espouse placing surgical clips across the sympathetic trunk as a means of blocking transmission of nerve signals. This technique is said to be as effective as cutting the trunk, and if the side effects of the surgery are intolerable to the patient, removal of the clips restores function to the presurgery state. Pancoast (Superior Sulcus) Tumor and
Syndrome
You will recall that the apex of the lung rises as high as the neck of the first rib. The ventral
ramus of T1 crosses in front of the neck of the first rib (hence behind the apex of the lung) to
reach the superior surface of the rib just posterior to the subclavian artery. At this site, the ventral
ramus of T1 is joined by the ventral ramus of C8 to form the inferior trunk of the brachial plexus.
You should also recall that lying on the head of the first rib is the first thoracic sympathetic
ganglion (called stellate ganglion if it is joined to the inferior cervical ganglion). From these
relationships you can deduce that tumors of the apex of the lung, particularly those located
posteriorly in the apex, may compress or involve the lower trunk of the brachial plexus and the
first thoracic sympathetic ganglion. Such tumors often produce pain (and later numbness and
weakness) in those regions of the upper limb served by C8 and T1. About 20% of the time a
Horner's syndrome is also produced [Detterbeck FC 1997 Pancoast (Superior Sulcus) Tumors.
Ann Thor Surg 63:1810-1818]. Tumors in the apex of the lung producing these symptoms are
called Pancoast tumors (after a radiologist named Henry Pancoast), and the suite of symptoms
due to nerve involvement are said to constitute a Pancoast syndrome. Although other diseases
involving the apex of the lung can produce a Pancoast syndrome, they are rare compared to
Pancoast tumor.
Repeated strenuous movements of the shoulder may lead to painful inflammation of the
subacromial bursa, or even injury to the rotator cuff muscles,
particularly supraspinatus. Furthermore, not everybody's scapula is shaped precisely the same.
Notably, the acromion process can be bent into a sort of hook. Orthopaedists classify acromions
according to how hooked they are.
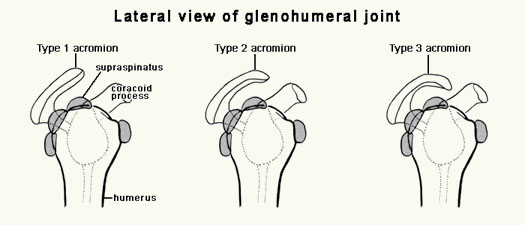
In older persons with arthritis of the shoulder, the intracapsular part of the biceps long head tendon may erode, so that the biceps long head then arises from the intertubercular sulcus of the humerus.
Winging of the Scapula
When the serratus anterior is paralyzed, the inferior angle of the scapula moves posteriorly
away from the chest wall to make a noticeable ridge beneath the skin of the back, a condition
known as winging of the scapula. Paralysis of the trapezius yields a similar change in appearance
of the back. At first look, the examiner may be unable to decide whether winging of the scapula
is due to a serratus anterior or a trapezius paralysis. The determination is then made by requiring
the patient to perform a motion for which one of the muscles is significantly more important than
the other. If that important muscle is damaged, the winging will become worse; if that important muscle is
intact, the winging will become less noticeable. For example, when the patient abducts the arm, a motion for which trapezius action on the scapula is particularly important,
trapezius-winging will become more prominent but a serratus-winging will lessen (or remain
unchanged). When the patient flexes the arm, a motion for which serratus action on the scapula is particularly important, a serratus-winging will worsen but any winging caused by a paralyzed trapezius will diminish.
The serratus anterior is not only a rotator of the scapula, but it also protracts (pulls anteriorly) this bone. Consequently, winging due to a paralyzed serratus anterior will be accentuated by applying a dorsally
directed force to the scapula that the paralyzed serratus is unable to resist. In diagnosis, this is
accomplished by asking the patient to hold his or her hands stretched out in front of the body and
then lean against a wall supported by the outstretched hands. This maneuver stresses the
protracting ability of the serratus and causes a serratus-winging to become even worse. Had the
appearance of winging at rest been due to a weak trapezius, the winging would virtually
disappear when the patient performed such a test. Posterolateral Thoracotomy
In the standard posterolateral thoracotomy, the serratus anterior is divided transversely. Many
surgeons prefer to make this cut lower than the intercostal space to be entered so as to preserve as
much as possible of the long thoracic nerve (nerve to serratus anterior).
Synovial Sheaths
A penetrating wound of a finger or thumb may introduce infectious material into its synovial digital flexor sheath. The sheath then provides a passageway for this infectious material to travel proximally into the palm. Because the synovial sheaths do not extend to the tips of the digits, wounds here run less risk of proximal spread of infection. The synovial sheath of the little finger is connected to the synovial bursa in the carpal tunnel. Consequently, an infection of the little finger's synovial sheath can spread into the carpal tunnel. Similarly, an infection of the thumb's synovial digital flexor sheath can spread into the carpal tunnel.
Muscle Interaction During Finger Flexion and Extension
This paragraph of Core Concepts states that contraction of an extrinsic finger extensor (EDC, extensor indicis, or extensor digiti minimi) by itself produces hyperextension at the MCP joint and, because of increased passive tension within the stretched FDP, flexion at the IP joints. This is true in the majority of persons, who require active contribution by some intrinsic hand muscles in order to straighten out their fingers. (A hand in which all the fingers are clawed is said to be intrinsic-minus.) However, in some people the ventral portion of an MCP joint capsule is so tight as to stop hyperextension of the joint. In such cases, an extrinsic finger extensor can fully extend the finger without any assistance from intrinsic hand muscles. Patients with tight ventral MCP joint capsules of the little and ring fingers will not present with the typical ulnar claw hand.
Superficial Ulnar Artery
Core Concepts states that injections meant for the median cubital vein may have dire consequences if put in a superficial ulnar artery. The reason is that solutions of drugs meant for intravenous injection are usually highly concentrated in anticipation of the fact that they will become diluted with venous blood from other parts of the body when they reach the heart. If such a solution is injected into an artery by mistake, it reaches the capillary bed of that artery without significant dilution. The result may be serious injury to capillary walls and to the tissues supplied by these capillaries.
Arterial Anastomoses in the Hand and the Modified Allen
Test (I wish to thank Scott McGovern, a Stony Brook medical student, for drawing my
attention to this Clinical Sidelight.)
In the hand there are two major anastomotic routes between the radial and ulnar arteries:
This issue has come to fore because (a) the radial artery is becoming increasingly popular as a substitute for the great saphenous vein during coronary artery bypass
grafting, (b) the radial artery is becoming increasingly popular as a substitute for the common femoral artery as the route for inserting the catheter needed to perform coronary angiography, (c) the radial artery is often cannulated for the purpose of monitoring blood pressure and blood gasses during anesthesia or in an ICU, and (d) hemodialysis usually involves
establishing an arteriovenous fistula between the radial artery and a vein at the wrist. Before
one removes the radial artery, or risks occluding it, or diverts its blood, it would be nice to know
if the patient's ulnar artery can take over complete supply of the hand, particularly of the thenar eminence and thumb, which rely most heavily on the radial artery for their supply of blood.
There are some sophisticated ways (measurement of blood pressure within the thumb, Doppler ultrasound measurement of blood flow in the princeps pollicis artery, pulse oximetry of the thumb) to assess the ability of the unlar artery to keep the entire hand alive, but many physicians recommend starting out with a very simple test called the modified Allen test. The examiner puts pressure on both the radial and ulnar arteries at the wrist, then either asks the patient to make and release a tight fist several times (YouTube Video), or to make a tight fist, hold it for 15 -30 seconds, then open the hand (YouTube Video). In either case, the making of the fist drives most of the blood out of the hand so that after the last opening, the palm and the palmar surfaces of the digits are pale. Now the real test begins. The examiner releases the pressure on the ulnar artery and observes if and how long it takes for the hand to turn red. If the collateral circulation between the ulnar and radial arteries is adequate, the hand will turn
from pale to red within 5 seconds even though the radial artery remains compressed. If it takes longer than 10
seconds to become red, then the ulnar artery is considered unable to supply the entire hand all by itself. Failure to turn red within 10 seconds is said to constitute a positive (or abnormal) Allen test. It is important that the patient be instructed not to overextend the wrist nor completely extend the digits, because doing so places tension on the skin and palmar aponeurosis
that may compress the cutaneous vessels and give a false positive result.
Many physicians believe that if a patient has a positive (abnormal) modified Allen test, you shouldn't perform any procedure on that patient that compromises the radial artery's blood supply to the hand. However, there is evidence that even when carefully done, modified Allen tests tend to give a fair number of false positive results. As a result, some physicians believe that in the case of a positive modified Allen test, the patient should undergo more sophisticated assessments of blood supply to the hand so as not to be excluded from a procedure on the radial artery that will actually be well tolerated.
The problem posed by the relatively high frequency of false positive modified Allen tests has recently been addressed by a paper proposing a new, but equally simple, method of assessing the ulnar artery's ability to supply the entire hand. This method uses a smartphone app able to measure blood circulation to the index finger (Di Santo P et al. 2018 Photoplethysmography using a smartphone application for assessment of ulnar artery patency: a randomized clinical trial. CMAJ 190:E380-E388). The app, called Instant Heart Rate (by Azumio), is available for both iPhones and Android phones. When the phone's camera lens is placed on the pad of one's index finger and the pad is illuminated by the camera light, the phone uses color and brightness changes of the reflected light to measure volume changes in the finger pad due to blood flow. While advertised as as a means to measure heart rate, the app also presents a graphical representation of blood volume change. When this graphical record is assessed during radial artery compression, a determination can be made of the how well the ulnar artery can take over blood supply to the index finger. This new method was found to be as good as the modified Allen test for detecting an inadequate collateral circulation to the hand, and to have many fewer false positive results than the modified Allen test. Time will tell if it becomes widely accepted.
Warm Ischemia Time
An organ or structure deprived of its blood supply will die. The length of time it can remain alive
at room temperature without irreversible tissue damage is called its "warm ischemia time". For limb muscles and nerves this is 4 hours (Whitesides TE Jr, Heckman MM. 1996 Acute compartment syndrome: update on diagnosis and treatment. J Am Acad Orthop Surg 4::209- 218). After 8 hours of warm ischemia, irreversible damage has occurred. In between these times, the damage is variable. If the affected segment is cooled to 4 °C the ischemic lifetime can be greatly extended (doubled or more). Major causes of limb ischemia are arterial occlusion and, more dramatically, accidental amputation.
As a result of these
anastomotic routes, if either the ulnar or radial artery is injured at the wrist, patients tolerate
ligation of the injured vessel very well. Does this mean you need not worry about damaging one
of these arteries during the course of another medical procedure?
(1) the superficial palmar arch, which in roughly a third of people is structurally complete (i.e., formed by a visible anastomosis between the superficial ulnar artery and the superficial palmar branch of the radial artery), and in another third of people is often called "complete" if the superficial ulnar artery sends a branch to the thumb but does not visibly connect to a branch of the radial artery;
(2) the deep palmar arch,
which is structurally a complete arch in almost everybody.
Suprascapular Nerve
The suprascapular nerve is not often injured by itself, although trauma to the posterior triangle of
the neck, or falls on the shoulder, may do so. In addition to the symptoms mentioned in this
chapter, right-handed persons usually experience difficulty in writing, since movement of the
hand across the page involves lateral rotation of the humerus.
Although a test of abduction
strength would reveal weakness of supraspinatus in the case of suprascapular nerve injury, the
examiner would be unable to distinguish this from weakness of deltoid due to axillary nerve
injury without further observations. Thus, the least ambiguous test for the suprascapular nerve is
for strength of lateral rotation of the arm. The patient is instructed to hold the arms at the sides
with the elbows flexed. The examiner attempts to push the hands inward against resistance by the
patient. The teres minor is too weak a lateral rotator to confound results of this test.
Subscapular Nerves
The subscapular nerves are rarely injured. One can theorize that such injury would greatly affect medial rotation of the arm, and also affect combined extension/adduction of the arm. The test for strength of medial rotation is to ask the patient to hold the arms at the side, with the elbows flexed, and then resist the attempt of the examiner to push the hands apart. If the patient is able to offer only weak resistance to this movement, and palpation of the pectoralis major indicates it is working, one can suspect injury to subscapular nerves. The test for strength of combined extension/adduction of the arm consists of asking the patient to hold the arm straight out to the side and resist the examiner's attempt to lift it upward and forward.
Axillary Nerve
The test for the axillary nerve consists of asking a patient to hold the arms straight out to the side while the examiner attempts to push them down. In this way, weakness of one deltoid relative to the other may be easily assessed. The motion will be weak if the supraspinatus is paralyzed, so one must use his/her powers of observation, or palpation, to determine that the weakness is due to a paralyzed deltoid.
Radial Nerve
Tests for motor function of the radial nerve consist of assessing strength of elbow extension,
wrist extension, and finger extension (at the MCP joint). Sensory examination involves choosing a spot of skin
whose innervation by the radial nerve is rarely, if ever, altered by variations in nerve distribution.
Such a spot is the web of skin overlying the 1st dorsal interosseous muscle on the back of the
hand. This skin is stimulated by soft and sharp objects to determine the patient's response.
Pectoral Nerves
Specific injuries to the pectoral nerves are rare. To assess function of the pectoral nerves, one asks the patient to hold the arms out in front of the body, and the examiner attempts to push the elbows apart against the patient's resistance.
Musculocutaneous Nerve
The musculocutaneous nerve is rarely injured alone. Fractures of the humerus, direct wounds to the axilla, or even axillary artery aneurysm may affect it. One must make sure not to damage the musculocutaneous nerve in an anterior approach to surgery on the shoulder. This is done by staying on the lateral side of the conjoint tendon of origin of coracobrachialis and short head of biceps brachii. The motor test for function of the musculocutaneous nerve is no more complicated than asking the patient to flex the elbow against resistance by the examiner.
Ulnar Nerve - How to Test
In routine physical examinations, assessment of the ulnar nerve is usually confined to one sensory and one motor test. The skin over the tip of the little finger is chosen for the sensory test, because its innervation by the ulnar nerve is rarely, if ever, altered by variations in nerve distribution. To assess ulnar-innervated muscles the patient is asked to spread apart his or her fingers while the examiner tries to squeeze the index and little fingers together. This tests the strength of the first dorsal interosseous and abductor digiti minimi (with flexor carpi ulnaris used as a synergist to prevent pisiform displacement).
Ulnar Nerve - Motor Symptoms If Damaged
It is stated that injury to the ulnar nerve at the wrist is characterized by clawing of the ring and little fingers. This is true in most people, but not in persons whose MCP joint capsules are so tight as to prevent hyperextension of the MCP joints. (I happen to be such a person.) In ulnar-nerve-injured patients with tight MCP joint capsules, the fingers can be completely extended by the extrinsic digital extensors. It is in this group (and in patients with high ulnar nerve injuries, where clawing is not so prominent anyway) that "falling away" of the little finger from the ring finger is most obvious. In Core Concepts, I describe this persistent abduction of the little finger (known as Wartenberg's sign) as being caused by paralysis of its palmar interosseous muscle. This is true, but another factor is needed to actually produce the abduction of the little finger. Most authors believe this factor is provided by tension within the tendon of extensor digiti minimi. In about half of people the extensor digiti minimi has an abductor leverage at the little finger MCP joint. Obviously, in the half of people in which the extensor digiti minimi cannot abduct the little finger, Wartenberg's sign is not a feature of ulnar nerve injury.
Median Nerve
In routine physical examinations, one motor and one sensory test for the median nerve are
performed. The motor test consists of asking the patient to make a circle by opposing the pads of
the thumb and little finger, whereupon the examiner attempts to pull the thumb away by applying
a force to its proximal phalanx. This is a test of strength for the thenar eminence muscles. The
sensory test consists of assessing cutaneous sensation at the tip of the index finger. This is the
part of the median's cutaneous distribution least susceptible to variation in nerve supply. Obviously,
other tests can be performed (e.g., of wrist flexion and finger flexion) if these two standard tests
produce suspicious results.
Quadrangular Space
During surgery on the shoulder from the anterior approach, one eventually reaches a point where the subscapularis must be transected. In so doing, the surgeon must take care not to extend the incision into the quadrangular space, wherein reside some important things.
Snuffbox
It is significant that the scaphoid is in the floor of the snuffbox, since fractures of the scaphoid are indicated by tenderness or swelling in the snuffbox.
De Quervain's Disease and Finkelstein's Test
(This section is being added at the suggestion of Jeffrey Jacobson, a Stony Brook medical student,
and with his help.)
As stated in Core Concepts 90, septa extend from the deep surface of the extensor
retinaculum of the wrist to the distal radius and ulna, thereby dividing the space beneath the retinaculum into compartments for the different
carpal and digital extensor tendons. Tendons of the abductor pollicis longus and extensor pollicis
brevis pass through the first, most radial, of these compartments, which lies along the lateral
aspect of the styloid process of the radius. Sometimes, for reasons unknown (but far more
commonly in women than in men), the retinacular tissue of this compartment becomes thickened,
thereby impinging upon the tendons passing beneath it. Movements of the thumb or wrist
produced by the APL and/or EPB then become painful. This state of affairs is called De
Quervain's disease. It may be accompanied by an inflammation of the synovial sheaths of the
APL and EPB tendons (i.e., tenosynovitis).
Finkelstein's test is used to determine if painful
motion of the thumb is from De Quervain's disease or has some other cause. The patient is
asked to make a fist, but one in which the fingers curl over the thumb, just as we were taught to avoid
when we were children. The examiner then grasps the hand and moves it into adduction (i.e.,
ulnar deviation) at the wrist. In De Quervain's disease, this maneuver causes severe pain over the
radial styloid process. One may also find a positive Finkelstein's test in arthritis of the first
carpometacarpal joint. These two conditions are then differentiated by pushing the first
metacarpal proximally while twisting it back and forth. Such a "grind test" elicits pain in pollical
CMC joint disease but not in De Quervain's disease.
Carpal tunnel syndrome is treated by surgical transection of the transverse carpal ligament. In the old days, a skin incision was made in the palm starting at a point just proximal to the projected position of the superficial palmar
arch and extending proximally to the distal carpal flexion crease. The incision was positioned along a line corresponding to the radial edge of the ring finger because this minimizes the chance of cutting the palmar cutaneous
branch of the median nerve which lies subcutaneously between the tendons of the palmaris longus and flexor carpi radialis. The transverse carpal ligament was cut near its ulnar attachment so as to minimize the possibility of damaging the median nerve.
Nowadays, unless contraindicated, surgery to incise the transverse carpal ligament is almost always done endoscopically and requires only a small transverse skin incision through one of the carpal flexion creases (again avoiding damage to the palmar cutaneous branch of the median nerve). There are a number of ways to perform the actual cutting of the ligament; two are shown in https://www.youtube.com/watch?v=B2HEQvBr03k and https://www.youtube.com/watch?v=OcCW064Gg6k&t=76s. Because the skin incision used in an endoscopic carpal tunnel release is small and does not go through the palm, recovery from surgery is much quicker and is associated with far less pain.
A human who sustains a minor fracture of the fibula will not generally require a cast because
the bone bears minimal loads.
Isolated injuries of the anterior cruciate ligament do occur, but there is no consensus on what
motion produces them. Excessive axial rotation, which involves injury to one of the collateral
ligaments, is often accompanied by an anterior cruciate tear. One
clinical test for the anterior cruciate ligament involves the examiner placing the knee of a supine
patient in 90° of flexion, then attempting to the pull the tibia forward off the
undersurface of the femur.

A more sensitive test for anterior cruciate injury is the Lachman test, but it requires greater skill to interpret. The difference is that the knee is placed is placed in only 20-30° of flexion. Now when the examiner tries to pull the tibia forward he or she will normally be able to elicit a few millimeters of movement, but this movement should have a firm stopping point. If the stopping point is "mushy", this is a sign of anterior cruciate ligament damage.
It possible for one bundle of the ACL to be injured while the other remains functionally intact, or the two bundles may both be injured but each at a different site along its length. If both bundles are seriously damaged, as is often the case, the entire ACL is replaced by a graft. There is an active debate about whether a single graft is sufficient or the surgeon should use two grafts, with each attempting to replicate the path of one bundle of the ACL. The "single-bundle" technique restores adequate resistance to anterior sliding of the tibia on the femur but, because the ACL also functions in stabilizing other motions at the knee, some orthopaedists believe that the more complicated "double-bundle" technique better reproduces the overall function of the ACL.
The posterior cruciate ligament is not as often injured as is the ACL. Isolated injuries of the PCL are usually the result of a posteriorly directed force applied to the proximal tibia when the knee is flexed. A classic example is an automobile passenger who, as the result of a car accident, is thrust forward so that the lower leg bangs into the dashboard. Falling down forward so that one lands on a flexed knee may also create the requisite force. The clinical test for the posterior cruciate ligament involves the examiner attempting to the push the flexed tibia backward off the undersurface of the femur. Virtually no motion is allowed in a normal knee; if significant movement does occur because of an injured posterior cruciate ligament, this constitutes a positive posterior drawer sign. The use of a double-bundle technique for repair of a seriously damaged PCL is even more controversial than use of this technique to treat ACL injuries.
A blow to the lateral aspect of the knee (not uncommon in football) may very well rupture
both the superficial and deep fibers of the medial collateral ligament. Because the latter are
adherent to the capsule, it and the attached medial meniscus may also be torn.
The lateral ligaments of the ankle are more frequently sprained than is the deltoid ligament.
A physician tests for the integrity of these ligaments by manually trying to move the foot in a way
that an intact ligament would resist. For example, the test for the anterior talofibular ligament is
for the examiner to place one hand on the front of the leg and then attempt to pull the foot
forward by pressure applied to the heel. If the foot can be pulled forward relative to the leg, this
is said to be a positive anterior drawer sign of the ankle, indicating a torn anterior talofibular
ligament.
Q Angle
In clinical practice, the Q angle is estimated by angle between two lines: one between the anterior superior iliac spine and the center of the patella, the other between the center of the patella and the tibial tuberosity. So estimated, the Q angle averages 13° in males and 16° in females. Lateral patellar dislocation occurs more often in women than men because of this difference, a reflection of women's higher femoral bicondylar angles.
Posterior Tibial Tendon Insufficiency (PTTI) ( I thank Matt Gotlin, a Stony Brook medical student, for drawing my attention to this condition.)
Some people are born with a predisposition to develop bilateral flat feet in childhood. This may be due to ligament laxity, or an underdeveloped sustentaculum tali, or other reasons I don't fully understand. However, unilateral development of a flat foot in an adult (called Adult Acquired Flatfoot Deformity, AAFD) is very frequently associated with degeneration or rupture of the tendon of the tibialis posterior muscle. Indeed some authors treat AAFD as if it were synonymous with PTTI. The tibialis posterior is an extrinsic muscle that provides support for the longitudinal arch. Although not active when a person is simply standing, the muscle comes into play during the stance phase of locomotion. It makes sense that if the muscle cannot do its job because its tendon has undergone a degenerative process or has ruptured, then the ligaments that support the longitudinal arch, particularly the spring ligament, are placed under greater stress and will eventually fail. However, there is a bit of the chicken and egg controversy surrounding the cause of AAFD. Some evidence exists that laxity of, or damage to, the spring ligament may precede the development of PTTI. The logic here is that ligamentous malfunction places extra stress on the tibialis posterior to serve as an active supporter of the arch, leading over time to PTTI. Regardless, people with AAFD usually show not only damage to the tibialis posterior tendon but also to the spring ligament (Deland JT et al. 2005 Posterior tibial tendon insufficiency: which ligaments are involved? Foot Ankle Intl 26:427-435). If AAFD has progressed beyond the point where it can be managed by conservative treatment, but has not yet reached the stage when correction can only be achieved by realigning and fusing ankle bones to one another, most experts believe surgical treatment should entail, among other things, an attempt to repair or reconstruct the spring ligament.
Plantaris
The very small plantaris muscle gives rise to a long thin tendon that is separate from the
Achilles tendon. It is a clinically significant structure for two reasons: (a) rupture of the plantaris
tendon is a highly painful condition, (b) the plantaris tendon may be removed to be used as a
graft for repair of badly damaged tendons in the hand.
Compartment Syndromes
The anterior tibial, peroneal, and deep posterior compartments of the calf are inexpansible.
Buildup of pressure within any of these compartments is a potentially serious problem because
the small veins in that compartment become compressed. As this happens, venous pressure rises and, consequently, the arteriovenous pressure gradient falls (Matsen FA III. 1980 Compartmental Syndromes. Grune & Stratton, NY). The result is diminished capillary flow and ischemia of the structures within the compartment. Nerves are most sensitive to such ischemia, and the first sign that compartmental pressure has
reached dangerous levels is tingling or diminished sensation in the areas of skin supplied by
intracompartmental nerves. Pain upon passive stretching of the involved muscles is also a sign
for concern. The compartmental ischemia leads to increased capillary permeability and further
swelling, so that the pressure buildup becomes increasingly worse. When the intracompartmental pressure rises to within 25 - 30 mm Hg of the average arterial pressure (diastolic + 1/3[systolic-diastolic]), capillary blood flow stops.
The diminished capillary blood flow of a compartment syndrome leads to tissue damage even before all capillary flow stops. If the high intracompartmental pressure goes untreated, all the compartmental contents will die. Muscles killed in this way become fibrotic and shortened. Not only are they nonfunctional, but the shortening results in deformities.
One cause of compartment syndrome is an unaccustomed period of strenuous exercise. Muscles become swollen and tender after such exercise. For muscles like the deltoid or pectoralis major, which are not within confined spaces, this swelling presents no particular problem and will resolve with time. If the overused muscles lie within an inexpansible compartment, such as found in the lower leg, it is still possible for the swelling to resolve itself without complication. However, it is also possible for the pressure buildup to lead to an "exertional" compartment syndrome. One example of this is anterior tibial syndrome, which may occur after a long walk by
an otherwise sedentary person. Anterior tibial syndrome (like any other compartment syndrome)
is accompanied by pain in the compartment. However, the first sign that intervention may be
necessary is malfunctioning of the deep peroneal nerve, revealed by tingling or diminished
sensation in the dorsal web of skin between the first and second toes. The treatment for this, and most other compartment syndromes, is to make a long incision through the fascia bounding the compartment. Such a "fasciotomy" relieves the intracompartmental pressure.
More common than exertional compartment syndromes are those that arise following trauma (like a broken bone) that causes
bleeding into the compartment. A third cause of compartment syndrome is reperfusion injury.
When a structure is deprived of blood, the capillaries become more permeable. If blood flow is
suddenly restored, the reperfused structure will swell. The general rule is that if a limb has been ischemic for 6 hours, whatever the reason, you should do a prophylactic fasciotomy prior to restoring
circulation. Obviously, if a limb has been ischemic for significantly more than six hours, it must
be amputated (see Warm Ischemia Time). Medial Tibial Stress Syndrome ("Shin
Splints")
The term "shin splints" has been applied to so many different conditions characterized by exertional leg pain (e.g., incipient anterior tibial syndrome, incipient deep posterior compartment syndrome, stress fracture) that most clinicians now advise against its use. However, it seems that the majority of
persons who present with what they believe to be shin splints are actually suffering from a
condition more properly called "medial tibial stress syndrome" (MTSS). The symptom of MTSS is a diffuse pain along the posteromedial border of the tibia, usually bridging the junction of its middle and distal thirds. This pain is brought about by exercise, most commonly running or jumping, and is to be distinguished from a stress fracture, the pain of which is more focal. At one time it was widely believed that MTSS was essentially an inflammation of the tibial periosteum (i.e., a periostitis) along the site where the medial edge of the soleus has a fascial attachment to the posteromedial edge of the tibia (below the actual origin of the soleus from the soleal line of the tibia). Among the appealing aspects of this theory was the increased incidence of MTSS in persons who experience an unusually high range (or possibly speed) of subtalar joint pronation during running. It is believed that such persons overuse the soleus, which is both a plantarflexor and supinator of the subtalar joint. Also, MRI on patients with posteromedial tibial pain frequently reveals periosteal edema in the affected region. The theory that MTSS is a periostitis even guides surgical treatment when more conservative approaches fail. The surgery primarily involves cutting the fascial attachment of the soleus to the posteromedial edge of the distal tibia. It does not always work.
The problem with attributing the pain of MTSS to periostitis is that most studies have found no evidence of periosteal inflammation in persons undergoing surgery for this condition. The pendulum is swinging toward the belief that basic pathology of MTSS is a decreased bone density (i.e., greater bone porosity) due to an incomplete remodeling effort as the bone attempts to respond to exceptionally high and/or frequent loads (Jones BH, et al. 1989 Exercise-induced stress fractures and stress reactions of bone: epidemiology, etiology, and classification. Exerc Sports Sci Rev 17:379-422). There is certainly evidence to support the existence of metabolic and histologic changes in the bone of the affected region. However, the link between having a zone of porous bone and being in pain is not clear (Gaeta M, et al. 2005 High resolution CT grading of tibial stress reaction in distance runners. AJR 187:789-793). It may be that the porous bone responds to heavy loading with microcracks that are painful, but the issue has yet to be resolved. One would like to reconcile the "porous bone" explanation of MTSS with a role for soleus overuse in causing this syndrome. The only suggestion of which I am aware is that contraction of the soleus may add to the bending loads on the tibia (Beck BR. 1998 Tibial stress injuries: an aetiological review for the purposes of guiding management. Sports Med 26:265-279).
Varicose Veins
Varicose superficial veins of the lower limb are not an uncommon result of pregnancy, since the enlarged uterus compresses the common iliac veins and thereby elevates venous pressure within the lower limb.
Great Saphenous Vein
Probably everyone knows that the great saphenous vein has particular clinical significance
for coronary bypass surgery. Being long and easily located, it is resected so that segments of it
may be used as grafts extending from the ascending aorta to various coronary arteries beyond the
sites of their occlusion. It also used for femoropopliteal bypass surgery (connecting the common
femoral artery to the popliteal artery so that blockage on the superficial femoral artery may be
bypassed). During femoropopliteal bypass, the great saphenous vein may be excised and turned
around so that the valves permit distal flow of blood, or it may be left in situ and all the valves
stripped out. If left in situ, its tributaries must be sutured so that arteriovenous fistulae do not
develop.
NOTE: For information on causes of injury to these nerves I
have relied heavily on the text Focal Peripheral Neuropathies by JD Stewart, 1993, Raven Press,
NY.
Femoral Nerve
The femoral nerve may be inadvertently cut during pelvic,
groin,
or hip surgeries. It may be stretched by a retractor during pelvic surgery. It may be compressed
against
the inguinal ligament during prolonged lithotomy position. Pelvic tumors, pelvic fractures,
anterior hip
dislocations, and penetrating injuries to the groin also place the nerve at risk. Motor tests require
the
patient to
extend the lower leg against resistance and, for the purpose of testing the rectus femoris and
iliopsoas, to flex the thigh against resistance.
Obturator Nerve
The anterior division of the obturator nerve is of particular clinical significance in the
symptomatic treatment of cerebral palsy. Children with this disorder may experience a severe
impairment of gait due to spastic medial rotation and adduction of the thigh. Transection of the
anterior division of the obturator nerve will paralyze gracilis, adductor longus, and adductor
brevis; such paralysis actually has a salutatory effect on locomotion. Elimination of spasticity in
the gracilis has the additional positive result of reducing the tendency of the knee to be held in a
partly flexed posture.
Like the femoral nerve, the obturator is not often injured. Intrapelvic tumors may compress
the obturator nerve. Sometimes the pressure exerted by the fetal head during parturition may
damage the maternal obturator nerve. Fracture of the superior pubic ramus, or hernia of bowel
through the obturator canal are other potential sources of injury. One tests for damage to the
obturator nerve by requiring the patient to adduct the thigh against resistance. Superior Gluteal Nerve
The Trendelenburg test is described in Core Concept 104. Another test for damage to the superior
gluteal nerve requires the patient to lie on his or her side and attempt to elevate the lower limb
against resistance.
Inferior Gluteal Nerve
The inferior gluteal nerve is tested by requiring the prone patient to flex the knee and then
raise the thigh off the examining table against resistance. The gluteus maximus should be palpated as the
test is performed. Flexion of the knee is necessary because it causes the hamstring muscles to
operate in unfavorable regions of their length-tension curves and, therefore, enables a purer test
of gluteus maximus strength.
Damage to the entire sciatic nerve may occur in major
traumatic injury to the buttock or thigh, fractures or dislocations of the hip, and during hip
surgery. Intrapelvic tumors and very poorly placed injections in the buttock can produce partial
injuries. Compression of the nerve can arise from sitting for a long time wedged in a toilet seat
(usually associated with inebriation), or in emaciated patients that lie supine on an operating table
for a long time, or during bicycling, or from prolonged sitting on one's thick wallet (usually
associated with being a professor). Paralysis of lower leg muscles supplied by both the common
peroneal and tibial nerves should cause one to think of damage to the sciatic, rather than separate
damage to its branches. Paralysis of the hamstrings is a sign of damage above the proximal thigh.
Some tests for motor function of the sciatic nerve are the same as those for its common
peroneal and tibial branches (see further on). However, assessing the strength of knee flexion addresses the sciatic's innervation of the hamstrings and short head of biceps femoris, branches to which are given off before the sciatic splits into the common peroneal and tibial nerves. So that the examiner can distinguish weakness of knee flexion due to sartorius or
gracilis paralysis from that due to muscles innervated by the sciatic nerve, palpation of the
hamstrings is essential.
Piriformis Syndrome
Many persons who experience sciatica (i.e., pain along some part of the distribution of the sciatic nerve) are found to have a slipped disc, but other patients with sciatica have myelograms or MRIs that show no evidence of disc (or other spinal) disease. After many years of debate, it is now believed that another common cause of sciatica is something called "piriformis syndrome" (Filler AG, et al. 2005 Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine 2:99-115). Folks with piriformis syndrome typically present with buttock pain that may or may not radiate down the back of the lower limb. When it does so radiate, it less commonly goes into the foot than in cases of disc disease. If it does go into the foot, the pain affects all five toes, whereas a radiculopathy due to a herniated disc affects only the toes innervated by the compressed spinal nerve (medial toes if L5, lateral toes if S1). Numbness and muscle weakness are rare in cases of piriformis syndrome, and the SLR (straight leg raise) test is usually negative. The pain is made worse by sitting, and also becomes worse when an examiner places the thigh in a flexed, adducted, and internally rotated position, especially if the patient is then asked to abduct or externally rotate the thigh against resistance. In its early stages, the pain of piriformis syndrome is believed to be caused by irritation of the sciatic nerve due to a spastically contracting piriformis muscle. Subsequently, the nerve may be affected by hypertrophy of the piriformis, or atrophy and tightness of the muscle, or secondary adhesions to the muscle and surrounding tissues. What initially causes spasm of a piriformis is uncertain, but it may be set off by a back injury or trauma to the buttock. Although a study of possible piriformis syndrome patients has been performed to see if visual abnormalities of the muscle or sciatic nerve can be detected by MRI, the best proof of the condition is that it is relieved either by MR guided injection of anesthetic and steroid into the muscle, or if this fails, by surgical resection of a segment of the piriformis overlying the sciatic nerve.
Tibial Nerve
The tibial nerve may be injured by wounds to the popliteal
fossa or back of the lower leg, fractures at the knee, or dislocations of the knee. It can be compressed by
a Baker's cyst, which is a fluid-filled pouch derived either from one of the bursae at the back of
the knee or from an outpocketing of synovial membrane through the posterior capsule of the
joint. Testing the motor functions of the tibial nerve is done by
requiring the patient to plantarflex the foot, to invert the foot, and to flex the toes against resistance.
Asking the patient to walk on his/her toes is another good test for the strength of the triceps
surae. Some physicians ask the patient to spread the toes apart in an attempt to assess the intrinsic
muscles of the foot, however, many of us perfect persons cannot perform this maneuver.
As stated in Core Concept 108, the common peroneal nerve is the most frequently injured nerve of
the lower limb. In addition to the listed causes of injury, plaster
casts, or the supports used to hold up the legs in the lithotomy position, can also compress the
nerve. Signs of injury are a combination of those resulting from
malfunctioning of both the deep and superficial peroneal nerves.
Specific motor test of the superficial peroneal nerve requires the patient to evert the foot
against resistance; the strength of this motion is due far more to lateral compartment muscles
than to peroneus tertius.
A specific test of the deep peroneal nerve requires the patient to dorsiflex the foot and toes against
resistance. Another test is to ask patient to walk on his or her heels, a behavior that requires strong anterior
tibial compartment muscles.
Common Femoral Artery
The ability to compress the common femoral artery against the head of the femur has
significance beyond taking the pulse of this vessel. Radiologists frequently use the common
femoral artery as a site to gain entry into the arterial system. A hypodermic needle is
inserted through the anterior wall of the vessel where it lies anterior to head of the
femur. A guide wire is threaded through the needle, the needle is withdrawn, a catheter is threaded over the guide wire into the artery, and finally the guide wire is withdrawn.
Catheters inserted in this manner may be
passed superiorly into the aorta or one of its branches for the purpose of angiography or selective arterial
embolization. At the end of the procedure, when the catheter is withdrawn, bleeding from the
common femoral artery is controlled by compressing it against the femoral head for 10 minutes. Following this compression, the patient must lie immobile for at least 2 hours to ensure cessation of external bleeding. If, by
mistake, the puncture needle had been directed too obliquely upward, with the result that it entered the
common femoral artery proximal to the femoral head or, worse, entered the external iliac
artery, one is left with a hole in a vessel that has no posterior structure against which it can be
compressed. The result may a considerable hematoma in the proximal thigh and/or pelvis. An example of this is found at
http://jackstern.org/RadiologySelfTest/indexanompath.html, case 7.
Some physicians prefer to perform a femoral stick by passing the needle through both the anterior and posterior walls of the artery, then partially withdrawing the needle so its opening lies in the arterial lumen. The site of arterial puncture should be the same as described above. If the puncture site is located too far distally, it may enter the superficial femoral artery where this vessel lies anterior to the superficial femoral vein. After piercing the back wall of the artery, the needle may inadvertently enter the vein, creating the risk that an arteriovenous fistula will develop.
The common femoral artery is large and provides a fairly direct route to the ascending aorta, but there are a few factors that mitigate against using the common femoral artery as the site of insertion for cardiac catheterization. In obese patients it is particularly difficult to hit the femoral artery. If a patient has advanced iliac atherosclerotic disease, this may hinder passage of the catheter into the abdominal aorta. As mentioned above, after the procedure is concluded the patient must remain supine and immobile for at least 2 hours, and if the stick was too high, internal bleeding is a real risk. For all these reasons, use of the radial artery as the insertion site for cardiac catheterization has grown in popularity. Though the radial artery is considerably smaller than the common femoral artery, it still may be easier to hit in an obese patient. In everyone, after the catheter has been withdrawn, external bleeding is easily controlled by a compression wrist band, allowing the patient immediately to walk and eat. Finally, there is no risk of internal bleeding from a radial artery stick. You will probably have deduced that the radial artery is not a suitable candidate for catheter insertion unless the hand can be kept alive by the ulnar artery during the period of the procedure. Hence performing an Allen test, or some more sophisticated assessment of blood supply to the hand, is a prerequisite. (I thank Derek Nelsen, a Stony Brook medical student, for alerting me to the increasing popularity of the radial artery as a site of insertion for cardiac catheterization.)
Sural Nerve
Posterior to the lateral malleolus lies the small saphenous vein, and posterior to the vein lies the sural nerve. The nerve is easily located here. It can be traced upward from this point and removed
virtually in its entirety to supply bridging segments during attempts to repair damage to more
important nerves of the body.
Uterine Cancer
It is generally true that pelvic organs drain to internal iliac nodes, but lymph from the fundus of the uterus and uterine tubes also drains via channels that accompany ovarian vessels back to lumbar nodes. As mentioned in Table 98, when the normal routes of uterine lymphatic drainage become blocked, lymph may drain through channels that accompany the round ligament through inguinal canal, and then to the superficial inguinal nodes. If the latter are sites of metastatic uterine cancer, this is a bad sign, because it implies that intrapelvic nodes are heavily loaded with tumor.
Tongue Cancer
Any region of the tongue near its midline will send lymph to both the ipsilateral and the contralateral sides. For example, the tip of the tongue drains to both right and left submental nodes, as well as directly to both right and left jugulo-omohyoid nodes. It is also the case that regions of the lower lip near the midline send lymph to both the ipsilateral and contralateral submental nodes. Consequently, paramedian cancer of the tongue or lower lip is far more serious than cancer of these structures' lateral edges, because of the potential for metastases to both the right and left deep cervical chains.
Sampling Axillary Nodes for Spread of Breast Cancer
Breast surgeons use a different terminology for naming groups of axillary nodes than do
anatomists. Surgeons usually speak of level 1 nodes, defined as those lateral to the
pectoralis minor muscle (i.e., the pectoral, subscapular, lateral, and a few central nodes),
level 2 nodes, defined as those deep to the pectoralis minor (i.e., most of the central nodes),
and level 3 nodes, defined as those medial to pectoralis minor (i.e., the apical axillary nodes).
The lower the number of the level, the more likely is the node group to be a recipient of mammary carcinoma
spread. (However, spread to level 2 nodes can occur with negative level 1 nodes and, although
unlikely, there can be positive level 3 nodes without tumor detected in either level 1 or level 2
nodes).
For obvious reasons, lymphatic drainage of the breast is the subject of much research. I summarize some of this research below, but even this summary contains far more detail than I would expect a first-year student to learn. I have highlighted in bold type what I think you should know.
Most surgeons accept that 75% of the lymph from the breast goes to the axillary nodes, while
25% goes to the internal mammary nodes (IMN). In fact, recent studies indicate that if breast cancer has spread to the axillary nodes, there is about a 25% chance it will also have spread to the IMN (Purushotham AD, Cariati M. 2005 Br. J. Surg. 92:131-132). On the other hand, among patients who have negative axillary nodes, only 5-15% (depending on the study) will prove to have tumor in the IMN. There is some indication that the superficial part of the breast drains almost entirely to axillary nodes, whereas the deeper portion drains to both the axillary nodes and the IMN (Shimazu K et al. 2003 Ann. Surg. 237:390-398). There is also some evidence that, although all quadrants of the breast send lymph to the IMN, the incidence of metastases to these nodes is somewhat higher if the tumor is in the medial half of the breast. Surgical sampling of lymph nodes draining the breast is generally confined to the axillary nodes, recognizing the pretty small chance of isolated IMN metastases and the greater difficulty of surgical access to the IMN.
One can identify the lymph node most likely to house metastatic breast cancer by combining a technique called lymphoscintigraphy with injection of a blue dye that is picked up by breast lymphatic vessels. Lymphoscintigraphy entails the injection of radiocolloid into the breast around the site of the tumor. After an hour or so, a blue dye is injected at the same site. An incision is made in the axilla and the surgeon looks for a lymph node that has picked up the blue dye and/or (using a Geiger counter) a lymph node that is radioactive. In either case, such a node is called a "sentinel node". Sometimes the blue node is also the radioactive node, sometimes they are different, sometimes there are two or three nodes that satisfy one or both of the criteria for being called a sentinel node. Regardless, a sentinel node is viewed as the first in the series of nodes that receives lymph from the breast. For many years after the development of the sentinel node procedure for breast cancer, the practice was to send identified sentinel nodes for immediate frozen section to determine if there were microscopic foci of tumor in these nodes. If tumor was found, the surgeon removed many more axillary nodes in a procedure simply referred to as an axillary node dissection. This was believed to improve survival rates and to help in planning future treatment.
Axillary node dissection is not without risks. Removing certain nodes along the axillary vein may interrupt lymphatic drainage from the upper limb. When lymphatic drainage from any region of the body wall is significantly blocked, that region tends to swell - a condition called lymphedema. Because breast lymph rarely goes to lymph nodes that lie along the convexity (i.e., superior surface) of the axillary vein, whereas most lymph from the upper limb goes to these nodes, breast surgeons will preserve them in hopes of minimizing the incidence of postoperative upper limb lymphedema. Also, crossing near the floor of the axilla is the intercostobrachial nerve. It is often sacrificed
during axillary node dissection, although in recent years surgeons are making a greater attempt to preserve this nerve because cutting it leaves the patient with unpleasant numbness on the posteromedial aspect of the upper arm. The surgeon should also look out for the thoracodorsal nerve, the nerve to serratus anterior (i.e., long thoracic n.), and the thoracodorsal artery. Preservation of the latter is especially important because the latissimus dorsi may be used later
for breast reconstruction.
To reach apical axillary nodes (level 3), which are usually only removed if there is to be a
mastectomy, the surgeon will cut ("take down") the pectoralis minor at its origin in order to
improve exposure of the relevant region. Effort should be made to preserve the medial pectoral
nerve, which often pierces the pectoralis minor. If this nerve is cut, the sternocostal pectoralis
major becomes atrophic.
Because an axillary node dissection may have undesirable consequences, and patients with microscopic tumor in a sentinel node will generally receive radiation and chemotherapy whether or not tumor has spread to other axillary nodes, a major study was conducted to determine if removal of numerous axillary nodes really helps (Giuliano AE et al. 2011 Axillary dissection vs. no axillary dissection in women with invasive breast cancer and sentinel node metastasis. A randomized clinical trial. JAMA 305:569-575). The findings were that axillary node dissection does not improve survival rates, or diminish rates of local tumor recurrence, in patients with positive sentinel nodes who received postoperative radiation and chemotherapy. As a result, many breast surgeons no longer send sentinel nodes for immediate frozen section. Instead, the removed sentinel nodes will be sent for standard pathological assessment over the next few days. The results guide details of future radiation and chemotherapy. However, axillary node dissections are usually still performed if the surgeon sees obvious tumor in axillary nodes.
As implied above, the overwhelming majority of sentinel nodes are found in the axilla. However, in a large series of patients with breast cancer, it was shown that about 15% of patients have sentinel nodes in both the axilla and the IMN (Hong J et al. 2005 Eur. J. Surg. Oncol. 31:942-948). (Other studies give higher percentages for sentinel nodes in both locations.) Only 2% of patients had a sentinel node in the IMN without having one in the axilla. There is active research on the value of attempting to identify metastatic disease in the IMN, but for the moment, standard procedure calls only for looking in the axilla to find sentinel nodes.
Variability in Lymphatic Drainage of the Skin (The new information presented below is my summary of Uren RF, Howman-Giles R, Thompson JF. 2003 Patterns of lymphatic drainage from the skin in patients with melanoma. J Nucl Med 44:570-582).
The figure accompanying Core Concept 111 depicts a human torso with one horizontal line drawn at the level of the clavicles and another at the level of the umbilicus. Arrows indicate the following: (1) lymphatic drainage from skin and subcutaneous tissue above the transclavicular plane goes to deep cervical nodes, (2) lymphatic drainage from skin and subcutaneous tissue between the transclavicular and transumbilical planes goes primarily to axillary nodes, but also to internal mammary nodes, and (3) lymphatic drainage from skin and subcutaneous tissue below the transumbilical plane goes to superficial inguinal nodes. These arrows also indicate that lymphatic drainage from skin and subcutaneous tissue to the right of the median sagittal plane goes to right-sided nodes, and lymphatic drainage from skin and subcutaneous tissue to the left of the median sagittal plane goes to left-sided nodes. All these "facts" are oversimplifications of the truth.
In cases of cutaneous melanoma it has become standard practice to look for sentinel nodes using lymphoscintigraphy (injection of radiocolloid into the skin around the site of the tumor) followed by imaging that reveals where radioactivity has concentrated. Observations have been made of drainage to lymph nodes in completely unexpected places, and in some cases to nodes not previously known to drain the skin. First, skin within a 10 cm region straddling either the transclavicular or transumbilical plane can drain to regions above that plane, below that plane, or both. Similarly, skin within a 10 cm region straddling the median sagittal plane can drain ipsilaterally, contralaterally, or both. Second, Uren and colleagues discovered that in 10-15% of patients the first nodes to drain skin of the back above the transumbilical plane are found in the triangular intermuscular space of the shoulder (i.e., that space bounded by teres major, teres minor, and long head of triceps brachii - see figure to Core Concept 90). This nodal group had not been previously known. Third, skin of the back in the vicinity of the transumbilical plane may drain to para-aortic nodes in addition to axillary or superficial inguinal nodes. For those of us who just want to memorize a simple pattern, the only good news is that drainage from the skin of the anterior trunk more often goes to predicted nodes, and less often crosses the midline, than lymphatic drainage from the back. The authors describe various other incidences of unexpected lymphatic drainage involving skin of the head and upper limbs. The bottom line is that one should memorize the lymphatic drainage patterns of the skin shown in the figure for Core Concept 111, but they are not chiseled in stone. Surgical Nomenclature for Nodes Draining the
Lungs
Surgeons use a nomenclature for lymph nodes draining the lungs that differs from
what you will find in most anatomy texts. The American Joint Committee on Cancer and the Prognostic Factors TNM Committee of the Union Internationale Contre le Cancer have adopted the scheme shown in the figure (modified from Mountain CF and Dresler CM. 1997 Regional lymph node classification for lung cancer staging. Chest 111:1718-1723). I have been told that a new standard nomenclature is in the works. Regardless, I cannot recommend that a first-year medical student commit this memory, except for a few terms I will mention below.

Also, one often hears the intrapulmonary nodes distal to the hilar nodes referred to as "peribronchial nodes". The hilar and peribronchial nodes are not accessible via mediastinoscopy without breaking the parietal pleura and risking pneumothorax.
The right lung drains almost entirely to right paratracheal nodes. The left upper lobe drains almost entirely to left paratracheal nodes. The left lower lobe drains to both right and left sides. If there is evidence of left lower lobe cancer, surgeons want to know if the cancer has spread to the right paratracheal nodes, because such spread is a counterindication for surgical treatment of the cancer. One way to get the necessary information is to perform a mediastinoscopy. Some facilities have supplanted this with a PET (Positron Emission Tomography) scan of the superior mediastinum, which is as sensitive, or more so, in revealing tumor involvement of relevant nodes. Finally, T. J. Santo, a student at Stony Brook, has drawn my attention to the existence of a relatively new technique - ultrasound guided transbronchial needle aspiration, in which a flexible bronchoscope fitted with an ultrasound transmitter/receiver and biopsy needle is passed into the trachea and mainstem bronchi, where the needle is jabbed through the wall of the air passageway to take cytologic samples from suspicious nodes identified on CT. This technique does give access to hilar and peribronchial nodes.
Iliac Node Dissection
When removing external iliac lymph nodes, the surgeon must be careful not to damage the genitofemoral nerve lying lateral to these nodes. When removing the obturator nodes, it is the obturator nerve that is in danger.
Cloquet's Node
Cloquet's node is variously described at the most superior of the deep inguinal nodes or the most inferior of external iliac nodes. It lies in the femoral ring (i.e., the entrance to the femoral canal). Deep inguinal nodes are sampled for spread of cancer from the lower limb, or from any superficial tissue below the umbilical plane. If Cloquet's node is negative, it is often considered unnecessary to go higher and sample external iliac and obturator nodes. If Cloquet's node is positive for cancer, the surgery is extended into the abdomen and pelvis to take out external iliac and obturator nodes.
Return to
Jack Stern's Home Page